Feasibility of a focal boost in MRI-guided online adaptive SBRT for locally advanced prostate cancer
PO-1941
Abstract
Feasibility of a focal boost in MRI-guided online adaptive SBRT for locally advanced prostate cancer
Authors: Mathijs Dassen1, Anja Betgen1, Peter De Ruiter1, Joeke Van Der Linden1, Lisa Wiersema1, Ben Neijndorff1, Tomas Janssen1, Leontien Abbenhuis2, Peter Van Kollenburg2, Casper Reijnen2, Linda Kerkmeijer2, Floris Pos1, Uulke Van Der Heide1, Ellen Brunenberg2
1The Netherlands Cancer Institute, Radiation Oncology, Amsterdam, The Netherlands; 2Radboud University Medical Center, Radiation Oncology, Nijmegen, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Recently, the FLAME trial showed that escalating dose to the intra-prostatic lesion(s) (IPLs) in patients treated with external beam radiotherapy for prostate carcinoma (PCa) can achieve excellent levels of biochemical control (92% at 5 years) in a high-risk population. In addition, the hypoFLAME 2.0 trial demonstrated the safety of focal dose-escalation in a hypo-fractionated treatment schedule of 5 fractions. The latter study, however, did not include patients with extensive seminal vesicle involvement and therefore safety of SBRT focal boosting for these patients could not be concluded. These patients pose a challenge in boosting, since the seminal vesicles are anatomically wedged between rectum and bladder and may show considerable geometric variations over the course of treatment. Therefore, the aim of this study was to determine the feasibility of delivering an integrated focal boost of >40 Gy to the IPLs in MRI-guided online adaptive SBRT for patients with locally advanced PCa with seminal vesicle invasion (T3b tumors).
Material and Methods
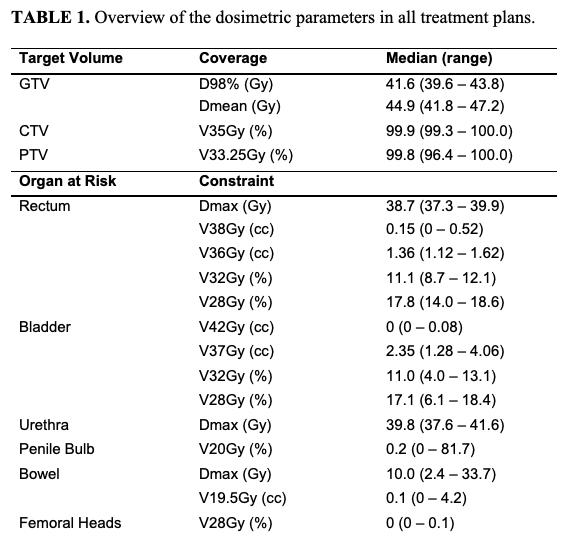
Data from 23 patients treated on the 1.5T Unity MR-Linac within the hypoFLAME 2.0 trial was used. MR images and delineations of target structures and organs at risk (OARs) were extracted from the clinically available data, which consisted of 5 adaptation MRI scans (one per fraction) including manually adjusted delineations. For the purpose of this study, the clinical GTV delineations were replaced by simulated GTVs of T3b tumors delineated by a radiation oncologist. Subsequently, the CTV was defined as the whole prostate including the seminal vesicles plus a margin of 3 mm around the GTV, excluding OARs. A PTV margin of 5 mm was applied. For each MR scan a treatment plan was generated by automated treatment planning using mCycle, simulating an online adaptive MRI-guided workflow. Patients were planned to receive at least 35 Gy to the CTV, with an isotoxic focal boost to the GTV up to 50 Gy. Planned dose distributions were analyzed by averaging dosimetric parameters over 5 fractions. In this way, analysis was robust for any large anatomical variations in single fractions.
Results
The planned D98% of the GTV showed a median of 41.6 Gy (39.6 - 43.8) and a GTV D98% of >40 Gy was achieved in 20 of the 23 patients. In 4 patients, a GTV D98% of >45 Gy could be planned for single fractions. The mean planned focal boost dose (Dmean) showed a median of 44.9 Gy (41.8 – 47.2). In all patients the V35Gy to the CTV was >99% and the V33.25Gy to the PTV did reach >99% in 17 of 23 patients. In 6 patients, PTV coverage was slightly reduced (but still at least 95%) either due to unfavorable filling of bladder and/or rectum or due to close proximity of the sigmoid colon. OARs constraints were met in all plans of all patients.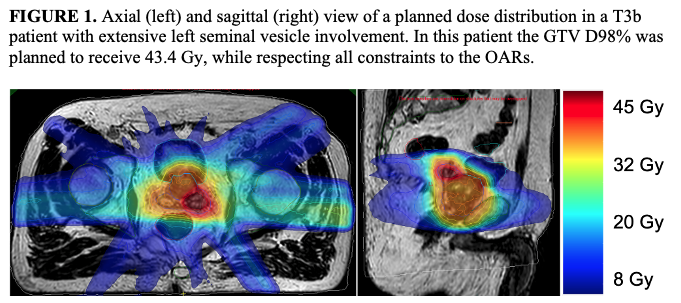
Conclusion
Focal dose-escalation of >40 Gy to the IPLs is feasible for locally advanced PCa using MR-guided online adaptive SBRT. Due to strict adherence to OARs constraints, a focal boost dose of >45 Gy was only reached in single fractions.