PBS proton therapy for neuroblastoma: dosimetric robustness to bowel gas variation
Allison Toltz,
United Kingdom
PO-1939
Abstract
PBS proton therapy for neuroblastoma: dosimetric robustness to bowel gas variation
Authors: Allison Toltz1,2, Steven J. Court3, Vasilis Rompokos1, J.E. Gains4, M.N. Gaze4, Y.-C. Chang4, P.S. Lim4,2
1University College London Hospitals, NHS Foundation Trust, Department of Radiotherapy Physics, London, United Kingdom; 2University College London, Department of Medical Physics and Biomedical Engineering, London, United Kingdom; 3University College London Hospitals, NHS Foundation Trust, Department of Radiotherapy Physics, London, United Kingdom; 4University College London Hospitals, NHS Foundation Trust, Department of Oncology, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
A challenge in proton therapy is in producing plans that are robust to anticipated changes in the patient anatomy. Small differences in the heterogeneities in the beam path between planning and treatment can produce large discrepancies in both target coverage and tissue sparing. Here we explore whether optimising directly on the overridden bowel structure may yield a plan that is overall more robust to interfractional bowel gas variation.
Material and Methods
Three cases previously treated with VMAT and exhibiting complex target volumes were selected: all comprised a midline target abutting both kidneys.
Our institutional guidelines for planning objectives (Rx 21 Gy in 14 fractions) and organ at risk constraints (V14Gy contralateral kidney < 10%) were used. Planning in Eclipse (PCS v15.6.05) followed the protocol of our previous work in which we investigated various beam arrangements and optimisation techniques. Each case was planned with single field optimisation and a three-field beam arrangement: an anterior field (included to try to improve kidney sparing) and two posterior oblique fields. The fields were optimised (NUPO v15.6.05) on the original bowel filling from the planning CT as well as two scenarios using manual overrides to simulate full (120 HU) and mean (-293 HU) over the bowel structure.
Weekly CBCTs were obtained for each case; three in total. Plans were then recalculated on the bowel filling from each CBCT (using manual HU overrides), and plan sums were created for evaluation.
Results
The planned target coverage and kidney dose for each optimisation scenario is compared to the recalculated target coverage on the plan sum from the weekly CBCT manual bowel filling overrides (Fig 1).
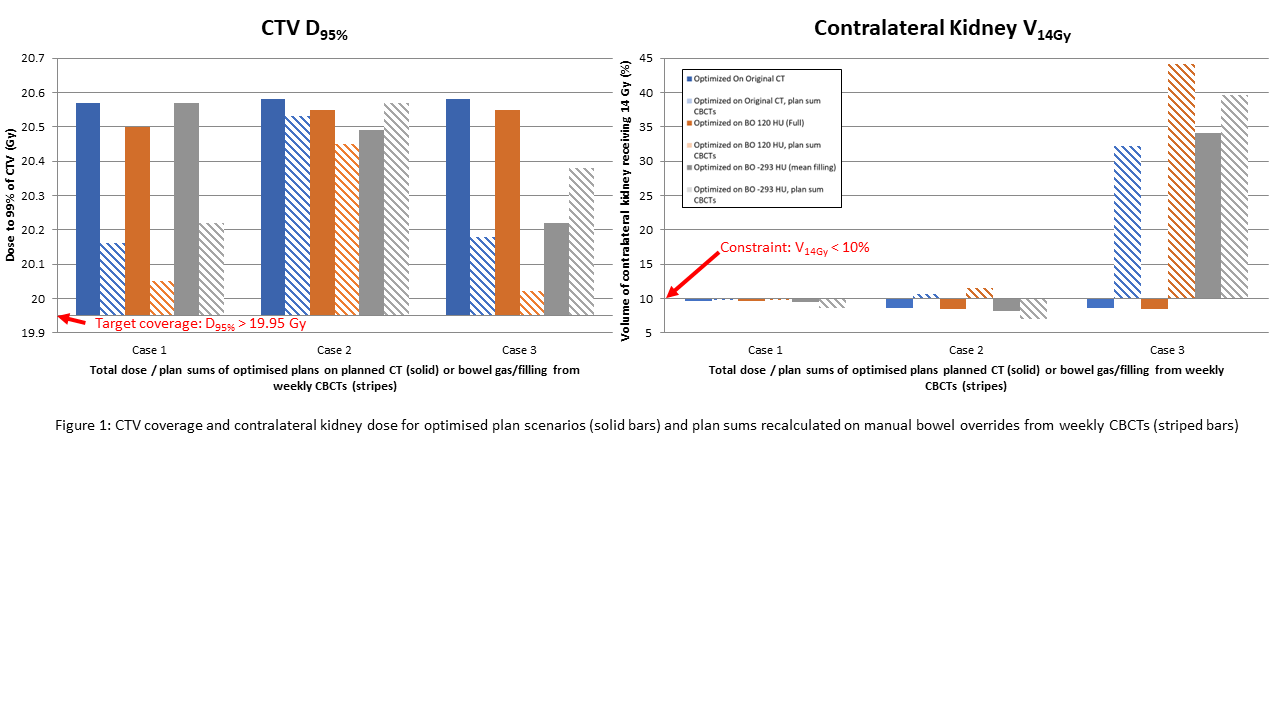
For all three patient cases, CTV coverage was maintained for the CBCT plan sums at the D95% for all the three planning scenarios. For Case 1, the contralateral kidney dose constraint (V14 Gy < 10%) was maintained for all CBCT plan sums. For Case 2, the contralateral kidney dose constraint was only maintained for the plan optimised on the mean bowel filling. For Case 3, contralateral kidney dose was exceeded for all three planning scenarios on plan sums.
Conclusion
The clinical cases with weekly CBCTs investigated retrospectively in the present work do not demonstrate a conclusive benefit in optimising plans on an overridden bowel structure to simulate variation in bowel filling. This work demonstrates all three methods of optimisation maintain CTV coverage on plan sums with manual HU bowel overrides from CBCTs but that kidney dose is sometimes significantly impacted regardless of optimisation technique.
The use of weekly CBCTs to estimate variation in bowel filling is a significant limitation of this study. As bowel gas present at planning simulation scan may not be representative of subsequent treatment anatomy, future work on an expanded cohort will continue investigating whether planning with a bowel override may result in a planning protocol consistently robust to bowel filling variation.