Planning target margins for CBCT guided radiotherapy of the breast/thoracic wall and lymph nodes
PO-1937
Abstract
Planning target margins for CBCT guided radiotherapy of the breast/thoracic wall and lymph nodes
Authors: Marianne Falk1, Mattias Hedman2,3, Mimmi-Caroline Bolin1, Jens Falk2, Kristin Karlsson1,3, Eva Onjukka1,3, Bruno Sorcini1, Giovanna Gagliardi1,3
1Karolinska University Hospital, Section of Radiotherapy and Engineering, Medical Radiation Physics and Nuclear Medicine, Stockholm, Sweden; 2Karolinska University Hospital, Department of Radiation Oncology, Stockholm, Sweden; 3Karolinska Institutet, Department of Oncology-Pathology, Stockholm, Sweden
Show Affiliations
Hide Affiliations
Purpose or Objective
The purpose of this study was to determine appropriate CTV to PTV margins for patients treated with adjuvant CBCT guided radiotherapy of the breast/thoracic wall and lymph nodes.
Material and Methods
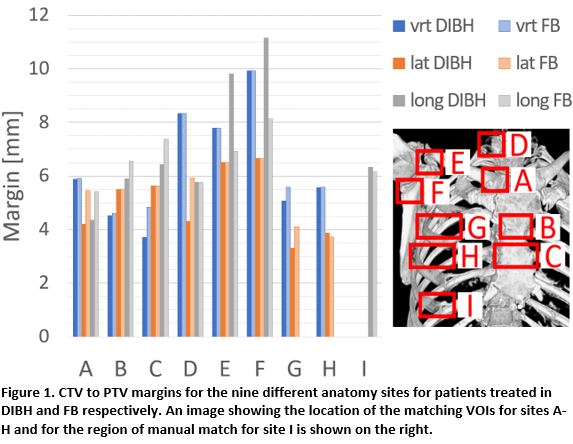
A total of 72 patients were enrolled in the study. Five of these were excluded as they had potential need of adaptation of their treatment plans due to set-up errors outside our clinics guidelines (7mm). Of the remaining 67 patients, 32 were treated in free breathing (FB) and 35 in deep inspiration breath-hold (DIBH). For three of the treatment fractions, CBCTs were acquired before and after the treatment and the setup uncertainties were evaluated by comparing the patient position at the time of treatment to that at the time of the CT acquisition for treatment planning. The intra-fractional uncertainties were evaluated by comparing images before and after the treatment. In addition, MV-imaging of a tangential treatment field was used to evaluate the setup uncertainties in the longitudinal (long) direction of the caudal part of the target as this anatomy was not visualized in the CBCT-image. Nine different anatomy sites were evaluated; (A) the proximal part of the clavicular bone next to the sternoclavicular joint, (B) the manubriosternal joint, (C) the middle of the sternum, (D) the proximal part of the vertebra C7, (E) the proximal coracoid process, (F) the proximal infraglenoid tubercle, (G) the proximal thoracic wall at the level of the manubriosternal joint, (H) the proximal thoracic wall at the level of the middle of the sternum and (I) the rib proximal to the caudal part of the target. Five patients received treatment of only the breast/thoracic wall and their images did not include the sites D-F. The image analysis was done in the Offline Review application of Aria 16 (Varian Medical Systems) using an automatic tool for matching with a VOI of 1.5 cm in the cranio-caudal (CC) direction for site A-H. Matching included translation in 3D, except for G-H where matching was done in vertical (vert) and lateral (lat) directions only, as these structures were too large to be properly identified in the long direction using a VOI of 1.5 cm in the CC direction. The MV-images were analyzed using manual match. Margins were calculated using the Van Herk margin formula ensuring 90% of patients receiving 95% of the prescribed dose. Statistical analysis of the difference in uncertainties in set-up and intra fraction motion for patients treated in FB and DIBH was done using a two-sided students t-test.
Results
For some anatomy sites and directions, there was no significant difference between the uncertainties in FB and DIBH treatments and a joint margin was calculated (table 1 and figure 1). The largest margins were calculated for D-F in the long and vrt directions.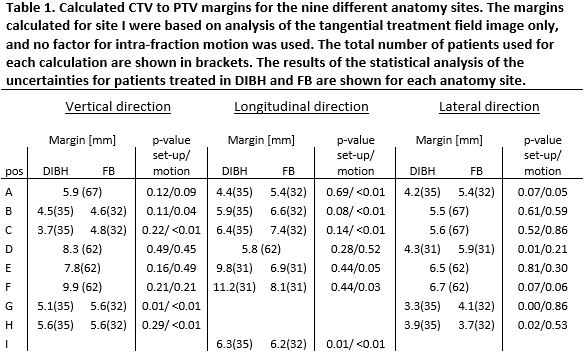
Conclusion
The results indicate potential benefit of asymmetrical margins for the cranial and caudal parts of the target, and that there is little difference between margins needed for FB and DIBH treatments, except for lymph node targets.