Clinical experience with robust VMAT optimization for breast and lymph node radiotherapy
Chrysi Papalazarou,
The Netherlands
PO-1935
Abstract
Clinical experience with robust VMAT optimization for breast and lymph node radiotherapy
Authors: Chrysi Papalazarou1, Koen Crama1, Ronald van der Slot1, Alice van Eijk2, Ellen van Reij1, Marcelle Immink1, Eleftheria Astreinidou1
1Leiden University Medical Center, Radiotherapy, Leiden, The Netherlands; 2Reinier de Graaf Gasthuis, Radiotherapy, Delft, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
To quantify the effectiveness and evaluate the parameters of a robust planning technique using clinical IGRT data.
Material and Methods
In January 2022 our department introduced a robust VMAT planning technique for breast/chest wall and lymph nodes irradiation, to a total dose of 40.05 Gy/53.4 Gy (SIB). The optimization includes a set of simulated CT’s that model breast deformation, as in [1]. We analyzed all cases in which a breast contour deviation was observed following local IGRT protocol. For consistency, we analyzed the original robust plan for all fractions, even in the cases when the plan was adapted during the series. CTV and PTV coverage of 95% of the elective dose was evaluated on the planning CT and on one of the simulated deformed CT’s (defCT’s) with a deviation of 8 mm in the lateral, inferior and anterior directions, corresponding to the action limit of the IGRT protocol. For each plan, 3 CBCT’s sampled from the treatment series (including those with maximum deviation) were imported in the TPS to evaluate CTV and PTV coverage during treatment, by deforming all relevant structures and recomputing the dose on an extended field-of-view CBCT. The dose of the missing fractions was estimated by applying random shifts to the closest available fraction image, based on locally collected intrafraction variation data (σ=2/3/4 mm for LR/IS/AP direction respectively). In contrast to Dunlop et al [2], our goal is not to establish the superiority of robust planning (here considered a given), but to quantify the extent to which the chosen robustness parameters are adequate for the clinically observed variation. Therefore, starting from a clinical constraint of a CTV D95%≥98% throughout treatment, we assess the number of false positives (replanning when CTV D95%≥98%, respectively), as well as false negatives (no action taken when CTV D95%<98%, respectively).
Results
Between January and September 2022, 93 patients received a robust VMAT plan. 13 cases (39 CBCT’s) were analyzed due to a deviation >8 mm during treatment. Means ± standard deviations of PTV V95% were: on the plan CT 98.3%±0.5%, on the defCTs 96.7%±1.3%; on the CBCT’s 91.8%±4.2%. Respective figures for CTV V95% were: 99.9%±0.1%; 99.5%±0.6%; and 98%±2.4%. See Fig. 1. In 9/13 cases, an adapted plan was made. On the basis of CTV D95%≥98%, we observed 3 false negatives and 8 false positives.
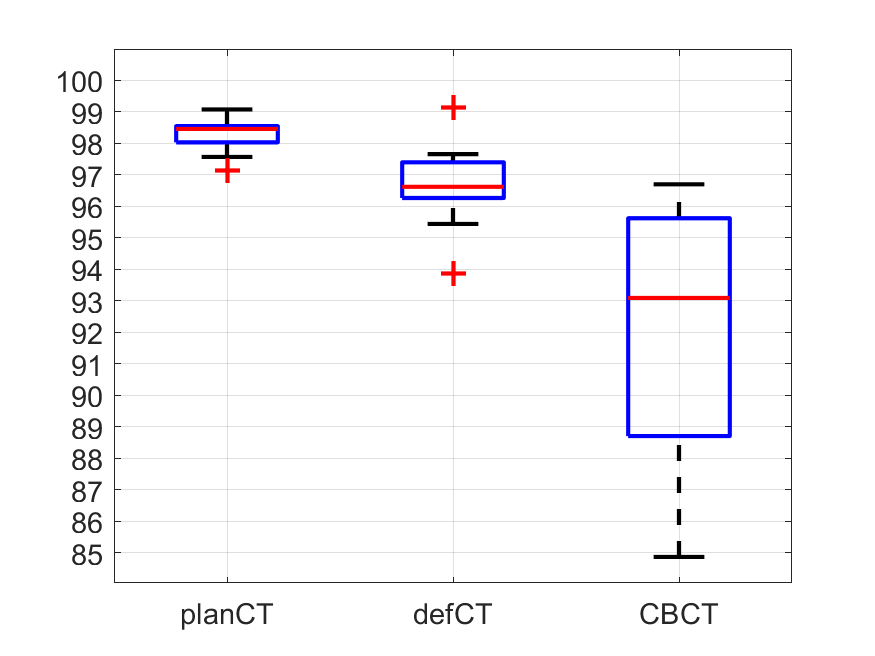
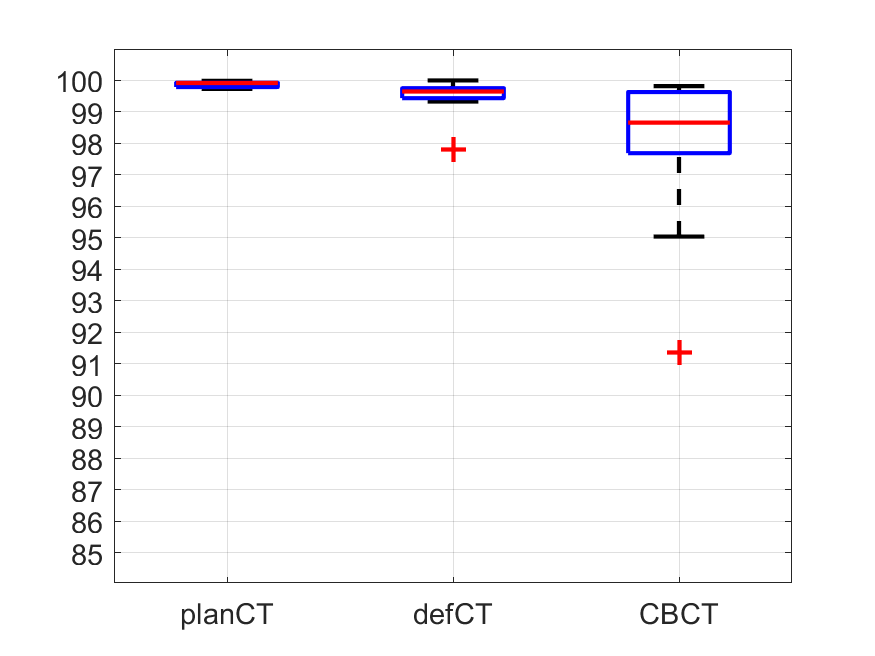
Figure 1: Boxplots of PTV (left) and CTV (right) V95%.
Conclusion
The robust optimization ensured CTV coverage throughout the treatment for 90/93 (96.8%) of patients. The high false positive rate suggests there may be room to adjust robustness parameters for higher conformality without losing robustness. However, the false negatives indicate that the robust optimization is unable to predict all plan deviations in practice, and therefore evaluation on the CBCT remains an indispensable clinical tool.
[1] K. Crama et al, Radiot & Oncol, pp. S1039-S1040, PO-1864, 2020.
[2] A. Dunlop et al, Clin. Transl. Rad. Onc., vol. 16, pp. 60-66, 2019.