A novel parameter to evaluate the dosimetric impact of Gastro-Intestinal gas pockets during MRgRT
PO-1929
Abstract
A novel parameter to evaluate the dosimetric impact of Gastro-Intestinal gas pockets during MRgRT
Authors: Matteo Nardini1, Matteo Galetto1, Amedeo Capotosti1, Luca Boldrini2, Giuditta Chiloiro2, Angela Romano2, Andrea Bevacqua2, Gabriele Turco2, Roberto Moretti1, Luca Indovina1, Lorenzo Placidi1
1Fondazione Policlinico Universitario ‘‘A. Gemelli’’ IRCCS, UOSD Fisica Medica e Radioprotezione, Roma, Italy; 2Fondazione Policlinico Universitario ‘‘A. Gemelli’’ IRCCS, UOC Radioterapia Oncologica, Roma, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Online adaptive radiotherapy has the potential to manage inter-fraction and intra-fraction motion either of organs at risk or targets, can also manage the anatomical changes causing electron density dissimilarities from simulation. The aim of this study is to evaluate the dosimetric impact of gastrointestinal (GI) gas pockets during online adaptive (OA) workflow in magnetic resonance guided radiotherapy (MRgRT) using a novel parameter called Active Gas Volume (AGV).
Material and Methods
CT scans of patients affected by upper GI tumours undergoing Magnetic Resonace guided Stereotactic Body Radiotherapy (MRgSBRT) were retrospectively evaluated. The analysis was performed by contouring the GI Organs at Risk (GIOARs), including stomach, small bowel, colon and gas pockets inside their lumen (GAS). The mean value of Hounsfield units (HU) for GAS structure of all patients was converted in ED (GIGED) using the calibration curve of our centre CT-scanner: 3 different treatment plans were calculated for each patient keeping all other plan parameters unchanged and forcing the GAS structure EDs with:
1-conventional AIR ED value
2-water ED value
3-GIGED value obtained in our study
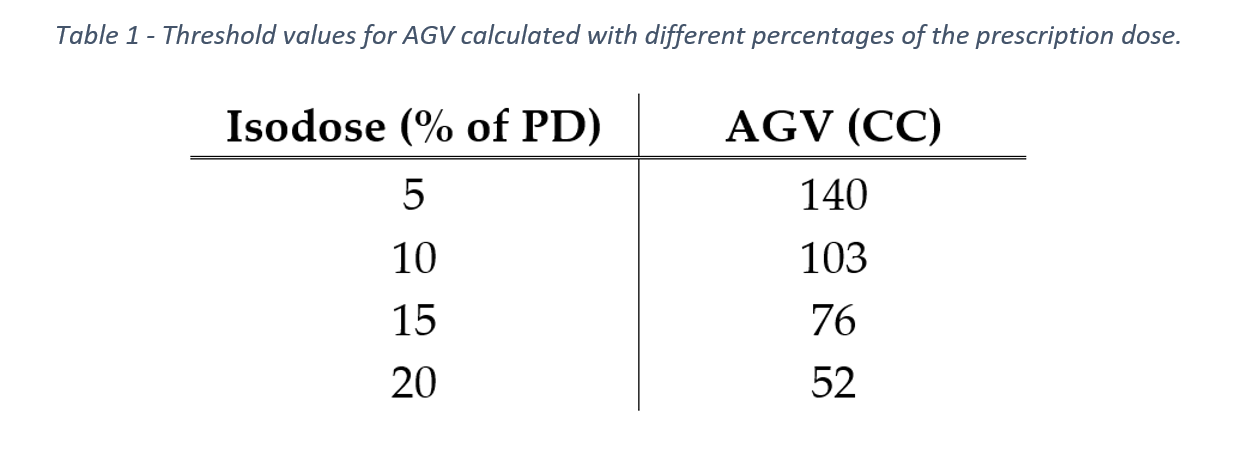
The dose distribution of the plan with the GAS structure ED forced with water ED represents the absence of gas pockets. Dose distribution for each plan was compared with others through gamma analysis. The Active Gas Volume (AGV) parameter was then calculated as the intersection of the GAS structure with the 5% isodose of the prescription dose to evaluate the volume of gas crossed by the beam path. In addition, the AGV was also calculated as the intersection of the GAS structure with 10%, 15% and 20% of prescription dose. In addition, we performed a measure of the variation of values extracted from the DVH for each type of plan. In particular, we considered: V95, D98, D2 and D50 for the planning target volume (PTV), D98, D50 and D2 of the GIOARs.
Results
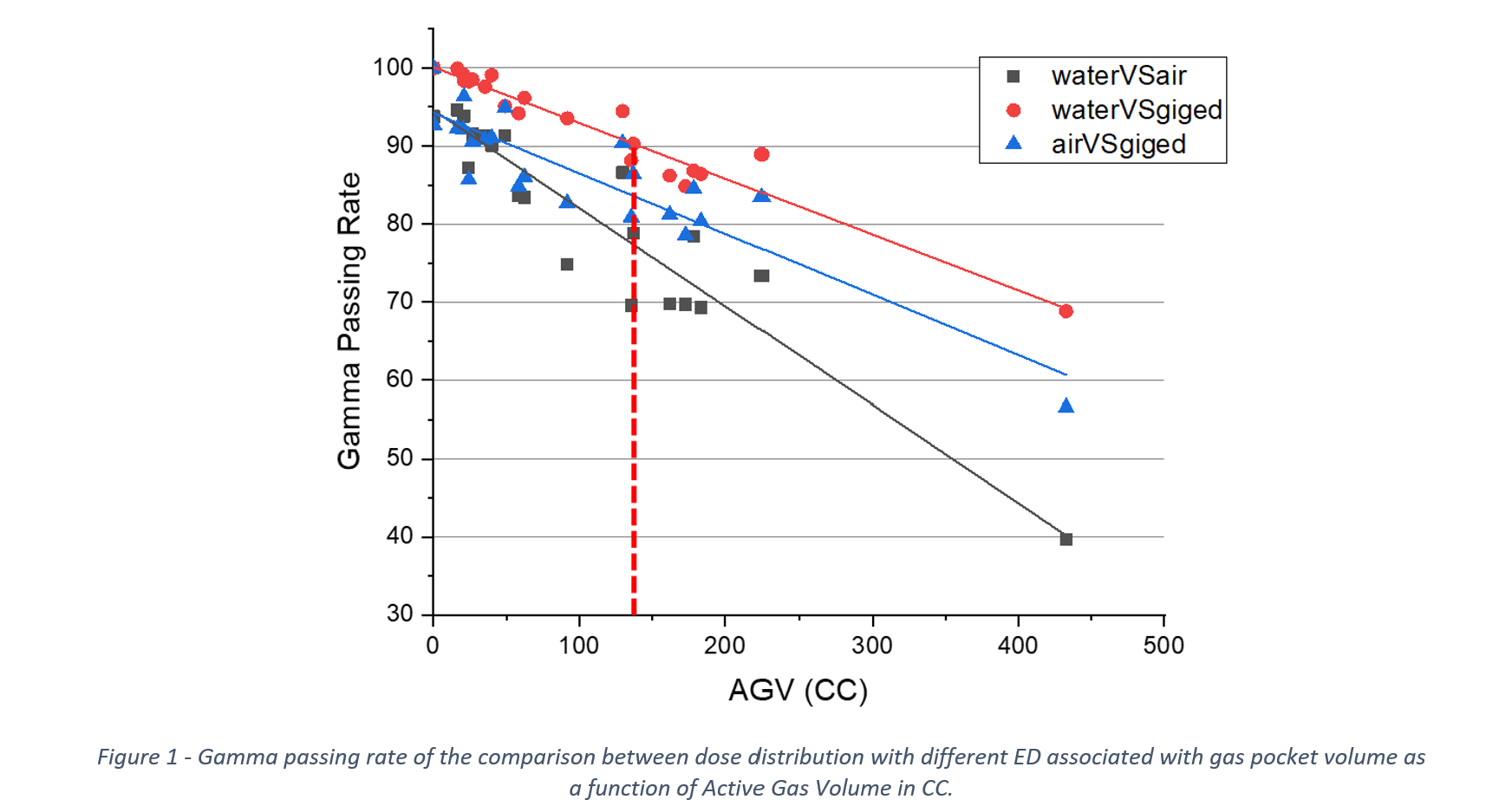
23 CT scans of 23 patients were evaluated for this analysis. The mean HU value of GAS structure is equal to -619.4 with an IQR of 116.5 corresponding to an ED of 0.38. No differences were found in the average values of HU depending on the organ at risk containing the gas pockets. Values of Gamma Passing Rate (GPR) in dose distributions’ comparison with conventional air ED and GIGED have been found to be inversely proportional to AGV. In particular, in the water VS GIGED comparison, GPR goes below 90% for values of AGV larger than 140 cc (Fig.1). Threshold values for AGV calculated with different percentages of the prescription dose are reported in Table 1. DVH analysis does not show gas pocket electronic density-dependent differences in dose values to organs at risk and targets.
Conclusion
Dosimetric impact of GI gas pockets depends on the AGV parameter. GI gas pockets cannot be disregarded in planning phase when the AGV parameter exceeds 140 cc. Adequate patient preparation is therefore suggested to reduce the AGV and make the replanning phase more straightforward.