Transit dosimetry analysis along lung cancer radiotherapy treatments for different treatment regimes
PO-1922
Abstract
Transit dosimetry analysis along lung cancer radiotherapy treatments for different treatment regimes
Authors: Alejandro Seoane1, Francesc Sansaloni1, Alejandro Campos1, Andrea Varó1
1Hospital Universitari Vall d'Hebron, Medical Physics, Barcelona, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
Lung cancer treatments are one of the most common sites where the tumour and/or organs at risk vary along the treatment, so replanning is required to adapt the initial plan to the new volumes.
Transit dosimetry measures the photon fluence passing through the patient body, so it is a powerful tool in detecting these anatomic variations and its influence in the dose distribution.
Different dose per fraction schemes are currently used, potentially leading to different volume variations along the treatment, so the aim of this work is to analyse the transit dosimetry for these different treatment regimes.
Material and Methods
Lung cancer patients treated from 02/2019 to 09/2020 with three different treatment schemes were included.
All of them were treated in a Varian Halcyon 2.0 linac with 6FFF MV (4 – 6 IMRT fields or 2 – 3 VMAT arcs), where transit dosimetry images are automatically acquired and stored for every treatment fraction. The first fraction image was set as the reference, and subsequent images were compared to the reference using Varian Portal Dosimetry v15.6 software. Comparison between the images was quantified by means of global gamma value with 3% - 3 mm parameters.
In case a patient required a replanning, the first fraction of the new plan was taken as the new reference image.
Mean gamma passing rate (GPR) along treatment fractions was studied for the three fractionations and for IMRT and VMAT techniques.
A Mann-Whitney U test was made to check the statistically significance to a 5% confidence level.
Results
A total of 62 patients and 3677 images were evaluated. Table I summarizes the patients, plans and fields analysed for the different schemes.
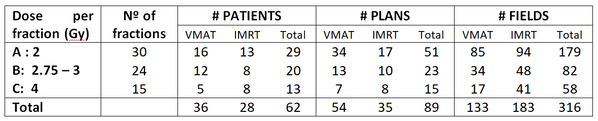
Figure 1.A represents the mean GPR for the patients treated in every fraction, stratified by the three treatment schemes. As expected, the GPR reduced along the treatment, being it more pronounced as the dose per fraction decreases.
The results of the statistical test among the treatment regimes showed statistical significance (p-values: p(A<>B) = 0.012; p(A<>C) < 0.001 and p(B<>C) = 0.001).
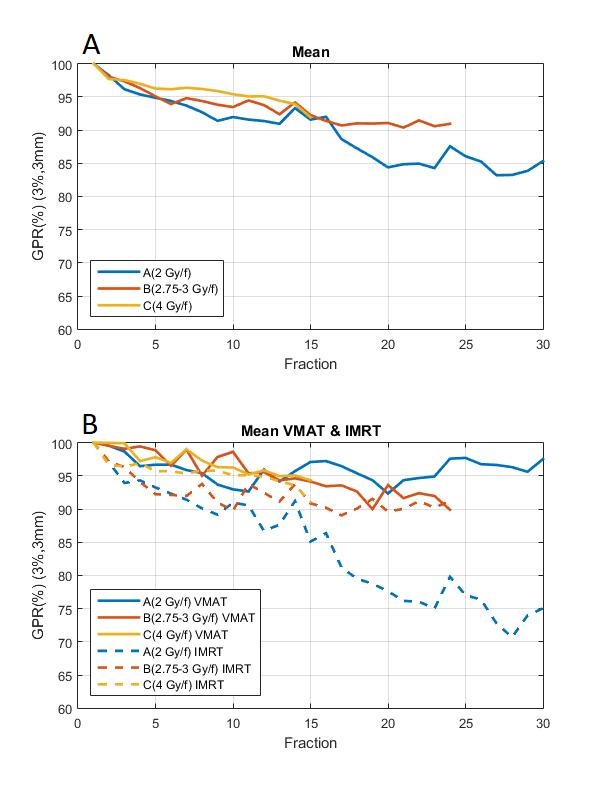
Figure 1.B shows it can be seen that in treatments with IMRT the values of GPR(%) are lower in all treatment schemes. As expected, the IMRT, having fixed gantry position, is more sensible to detect changes in the patient with portal dosimetry than VMAT, where the image is integrated throughout the entire gantry arc.
The results of the statistical test among the treatment techniques IMRT and VMAT showed statistical significance for treatment regimens A and B (p < 0.001), but not for the most hipofractionated treatment C (p = 0.065).
Conclusion
Portal transit dosimetry along lung cancer treatments revealed a different behaviour depending on the fractionation scheme. The results also depend on the treatment technique except for the most hypofractionated regime.
In view of these results, different protocols to check the patient variation along the treatment can be set based on the treatment dose scheme.