Serial exit dose fluence analysis to detect volume change and implication in adaptive radiotherapy
PO-1920
Abstract
Serial exit dose fluence analysis to detect volume change and implication in adaptive radiotherapy
Authors: Arnav Tiwari1,2, V.P. Pandey2, Vipin Kharade2, Rajesh Pasricha2, Manish Gupta2, Saikat Das2
1Postgraduate Institute of Medical Education and Research, Radiotherapy and Clinical Oncology, Chandigarh, India; 2All India Institute of Medical Sciences, Bhopal, Radiation Oncology, Bhopal, India
Show Affiliations
Hide Affiliations
Purpose or Objective
Decisions on adaptive radiotherapy depend on the patient, tumor, and treatment-related factors. Objective parameters for adaptive replanning are sparse. The present study reports tumor volume variation during high-precision radiotherapy and serial exit dose measurement as a patient-specific tool for adaptive radiotherapy.
Material and Methods
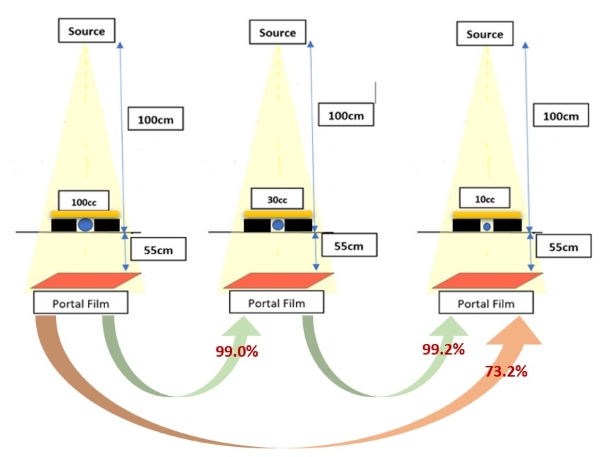
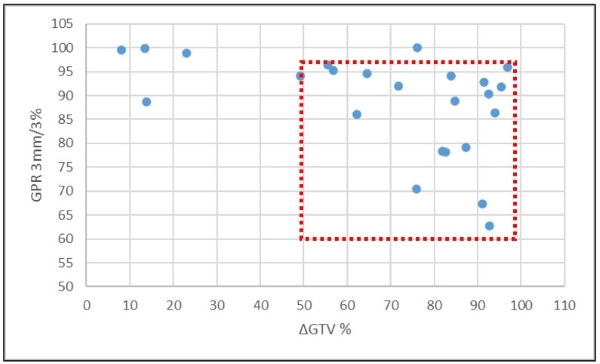
Three simulated tumor models were made using water-filled balloons of 100cc, 30cc, and 10cc each to simulate tumor shrinkage. Each model was planned for a 2 Gy dose based on a 100cc tumor placed at 100cm SAD. The dose was delivered, and the exit dose was calculated using Gafchromic films at 155cm SSD. The films were digitalized for Gamma analysis between the films. Secondly, serial exit dose fluence of 24 patients with a gross disease undergoing IMRT/VMAT treatment were measured. Baseline and mid-treatment exit dose registration was done using gafchromic films placed at SSD of 155cm in a predefined region of interest. The two exit dose films were compared after digitalization with gamma pass rate (GPR). The difference in the volume of GTV at baseline (from simulation CT scan) and mid-treatment CBCT scan was calculated (∆GTV).
Results
Comparing the exit dose fluence of simulated tumor models showed that there is no major change in exit dose fluence on reducing the volume from 100cc to 30cc (30%) or 30cc to 10cc (33%) with GPR of 99% and 99.2%, respectively. There was a large difference for volume change from 100cc to 10cc (90%) with a GPR of 73.2%.
Mean tumor volume was 83.7cc and 38.8cc in baseline and mid-treatment scans. On the serial measurement of exit dose, fluence tumor shrinkage significantly influenced the gamma pass rate. The mean gamma pass rate was significantly different between groups with and without 50% tumor volume shrinkage (86.36 vs. 96.24, p=0.008). On multivariate analysis with Gamma pass rate as a dependent variable and percent change of primary tumor volume and mean radial error as an independent variable significant relationship was found between ΔGTV and GPR (p=0.026)
Conclusion
Serial measurement of exit dose fluence by radiochromic film is a feasible method of exit dose comparison in IMRT/VMAT, where EPID dosimetry is not available with linear accelerator configuration. Our study suggests that a significant reduction in tumor volume (>50%) can be predicted with exit dose fluence comparison and thus provides an objective method to assess the requirement for adaptive radiotherapy treatment planning.