SBRT for central lung lesions: large biological delivered dose deviations for the bronchi
PO-1919
Abstract
SBRT for central lung lesions: large biological delivered dose deviations for the bronchi
Authors: Elias Lindbäck1,2, Karam Al Jirf3, Lone Hoffmann4,5, Ditte Sloth Møller4,5, Kristin Karlsson1,2, Simon Nyberg Thomsen4,5, Karin Lindberg2,3, Azza Ahmed Khalil4,5, Julien Uzan6, Eva Onjukka1,2
1Karolinska University Hospital, Department of Medical Radiation Physics and Nuclear Medicine, Stockholm, Sweden; 2Karolinska Institute, Department of Oncology and Pathology, Stockholm, Sweden; 3Karolinska University Hospital, Department of Cancer, Stockholm, Sweden; 4Aarhus University, Department of Clinical Medicine, Aarhus, Denmark; 5Aarhus University Hospital, Department of Oncology, Aarhus, Denmark; 6Raysearch, Service, Stockholm, Sweden
Show Affiliations
Hide Affiliations
Purpose or Objective
Stereotactic Body Radiation Therapy (SBRT) for centrally located lung lesions is associated with the risk of fatal bleeding, potentially resulting from damage to the main and intermediate bronchi, hereafter referred to as bronchi. When studying dose response of thoracic organs at risk (OAR), considering uncertainties in dose from the breathing motion and heterogenous hypofractionated dose distributions is important. The current study estimates the relative contribution from breathing motion and set-up deviations, respectively, to the uncertainty in dose to the bronchi, based on 4DCT phase images and CBCT images.
Material and Methods
Thirteen patients treated for central lung tumours were retrospectively included and imported into RayStation 12A-R; median [IQR] of the GTV to bronchi distance was 6 [2 – 18] mm. The periphery of the planning target volume (PTV) was prescribed 7 Gy x 8, corresponding to 14 Gy/fraction in EQD2 (α/β = 3 Gy). Typically, the maximum dose was around 150%. Treatment plans were created on a separate free breathing treatment planning CT (TPCT). Bronchi were delineated on each online tumour-match CBCT and each of the eight (or ten) 4DCT phase images by an oncologist. Original treatment plans were created in Eclipse, but dose distributions were recalculated in RayStation on the TPCT, CBCT and 4DCT phase images, based on online match position and DICOM frame of reference, respectively.
The bronchi DVH for each image dose was exported and converted to EQD2 (α/β = 3 Gy). D0.1cc values were compared to the planned dose in EQD2 for all image doses. The hypothesis of equal magnitude of this deviation in D0.1cc, comparing CBCT and 4DCT, was tested in a Mann-Whitney U test.
Results
The absolute median difference in D0.1cc (EQD2) was 1.13 [0.14 – 2.48] Gy3 and 0.72 [0.32 – 1.64] Gy3 for 4DCT and CBCT doses, respectively, which was not statistically different (p=0.69). However, considering each patient individually, the range of deviations was generally smaller for 4DCT than CBCT (Figure 1 and Figure 2). On a cohort level the deviation for the 4DCT could be affected by a TPCT acquisition in a non-representative breathing phase for a few patients.
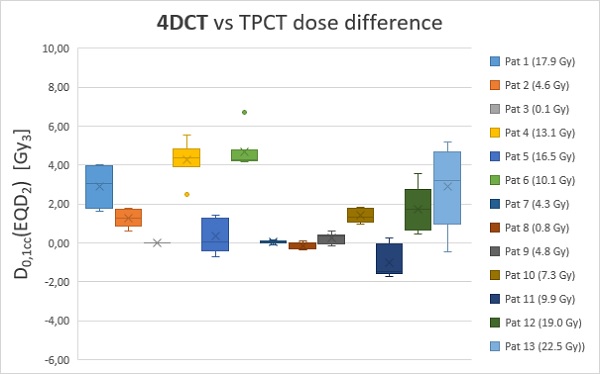
Figure 1: 4DCT vs TPCT dose differences and deviation from planned dose in EQD2, planned doses to bronchi for each patient is reported in the legend (Gy3). Each box consists of eight (or ten) data points
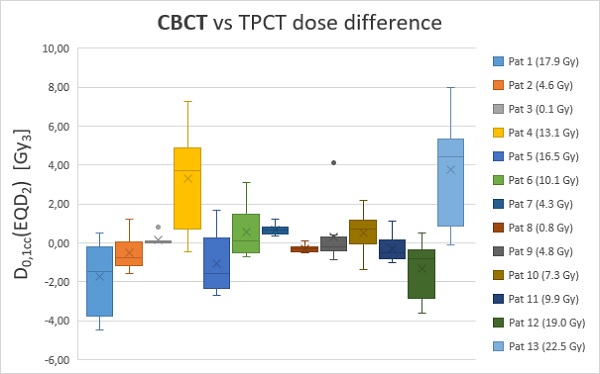
Figure 2: CBCT vs TPCT dose differences and deviation from planned dose in EQD2, planned doses to bronchi for each patient is reported in the legend (Gy3). Each box consists of eight data points
Conclusion
Hypofractionated and in-homogenous dose distributions can lead to large deviations in ‘biological’ delivered doses to the bronchi. When comparing the effect on the dose deviation for bronchi, related to breathing motion and set-up deviations, respectively, these are of similar magnitude in the cohort.