Stability assessment of patient-specific 4DCT and 4DCBCT correspondence models
PO-1917
Abstract
Stability assessment of patient-specific 4DCT and 4DCBCT correspondence models
Authors: Laura Büttgen1, Lukas Wimmert2, Frederic Madesta2, Rene Werner2, Tobias Gauer1
1University Medical Center Hamburg- Eppendorf , Radiotherapy and Radiation Oncology, Hamburg, Germany; 2University Medical Center Hamburg- Eppendorf , Institute for Computational Neuroscience, Hamburg, Germany
Show Affiliations
Hide Affiliations
Purpose or Objective
ITV-based SBRT strongly relies on a stable correlation between external breathing signal and internal tumour motion over the course of treatment. A workflow is proposed to assess the stability of patient-specific correspondence models using repeated 4DCT and pre-treatment 4DCBCT data.
Material and Methods
Based on 60 patients with both 10-phase planning 4DCT (Siemens AS Open) and 10-phase pre-treatment 4DCBCT (Varian TrueBeam v2.7), a representative subset of 6 patients was selected with regard to tumor visibility, range of tumor motion, 4DCBCT image quality etc. Due to sub-optimal 4DCBCT image quality for correspondence modeling, a set of 3 patients with repeated 4DCT scans (lung tumor, good tumor visibility, SI tumor motion >5mm) were included into the study to avoid bias in the proposed workflow. For each 4D data set (initial planning 4DCT and subsequent repeated 4DCT/pre-treatment 4DCBCT), correspondence models were built using most stable maximum exhale breathing phase. Via rigid registration between the maximum exhale image phase, the GTV target volume was transferred from the planning 4DCT to the subsequent repeated 4DCT and 4DCBCT, respectively. GTV volumes in the planning 4DCT of each breathing phase were predicted using the external patient breathing signals recorded during 4DCT by the Varian RPM system. Predicted GTVs and the surrounding ITV were compared with the initial GTVs/ITV using the dice similarity coefficient (DSC). DSC values were correlated with patient-specific prognostic parameters (breathing characteristics; GTV, ITV, lung volumes).
Results
Assessment of correspondence models stability between planning 4DCT and pre-treatment 4DCBCT resulted in mean GTV-based DSC of 0.72 ± 0.11. The respective ITV-based DSC was higher for all patients and fractions (mean DSC of 0.82 ± 0.04). With regard to the impact of 4DCBCT image quality, assessment of correspondence model stability between planning 4DCT and repeated 4DCT leads to an average GTV-based DSC of 0.82 ± 0.04 and an ITV-based DSC of 0.86 ±0.05, respectively. 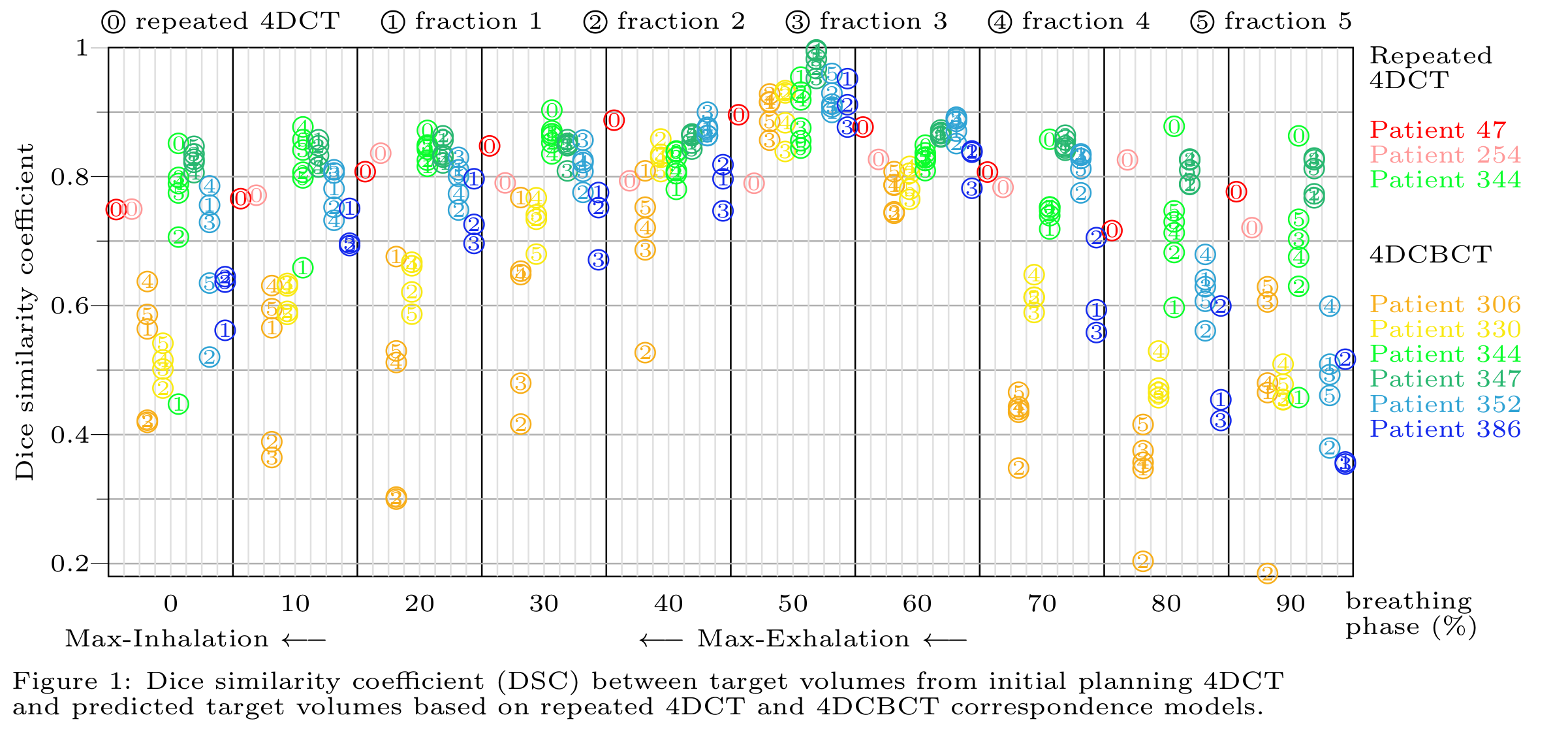
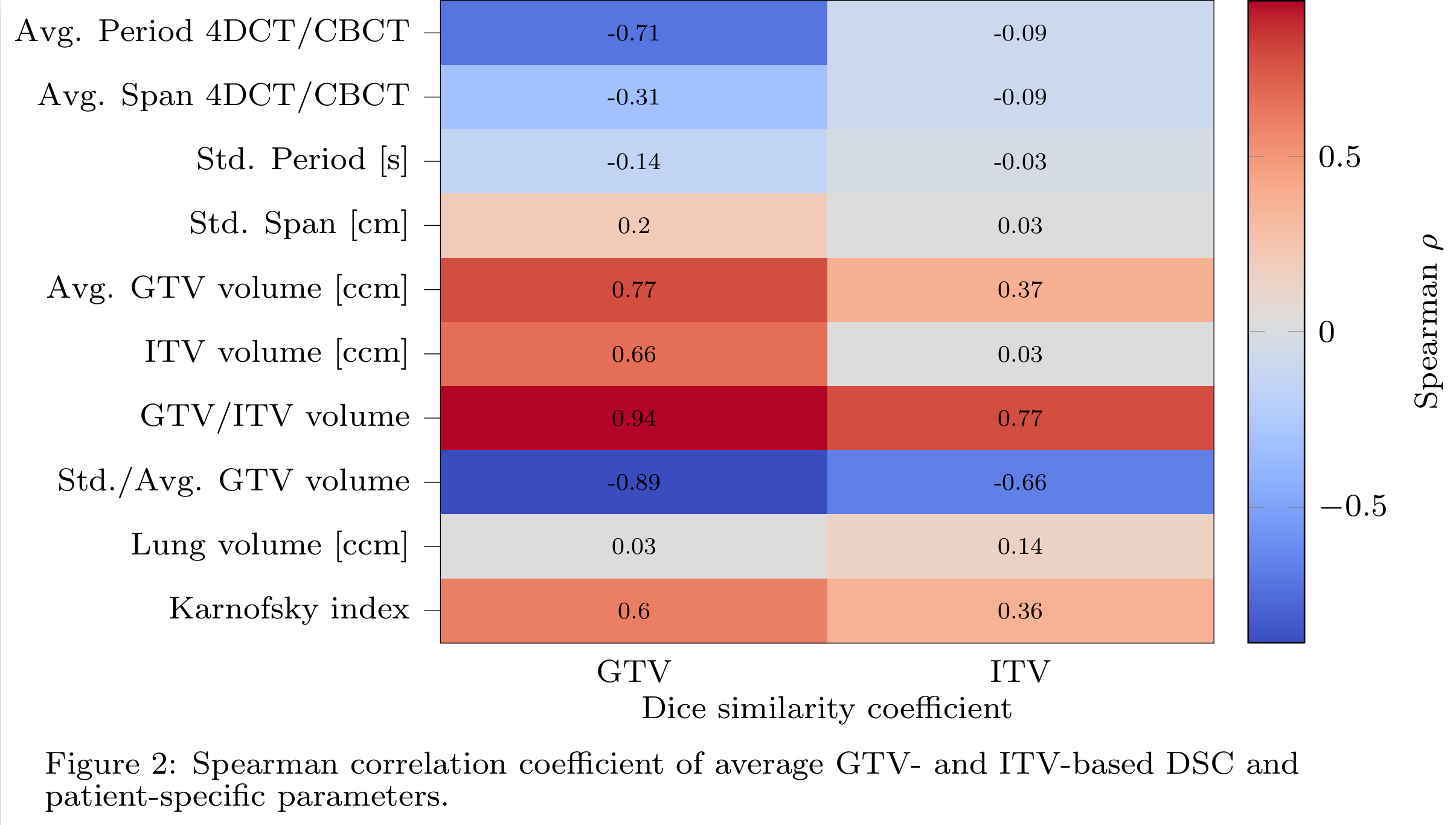
As presented in Fig. 1, the GTV-based DSC of each breathing phase decreased when approaching maximum inhale phase (0%). Stark variability of DSC values of various fractions indicates differences of planning 4DCT and pre-treatment 4DCBCT correspondence models for 2 patients (306, 344). Correlation coefficients of GTV/ITV-based DSC with prognostic clinical parameters are summarized in Fig. 2. A strong correlation was found for the GTV/ITV ratio, which is per definition the tumor motion range.
Conclusion
The proposed workflow allows for patient-specific assessment of correspondence models stability over the course of treatment and to identify patients that would benefit from adaptive re-planning. Corresponding DSC thresholds (e.g. >0.7) need to be confirmed using a larger cohort.