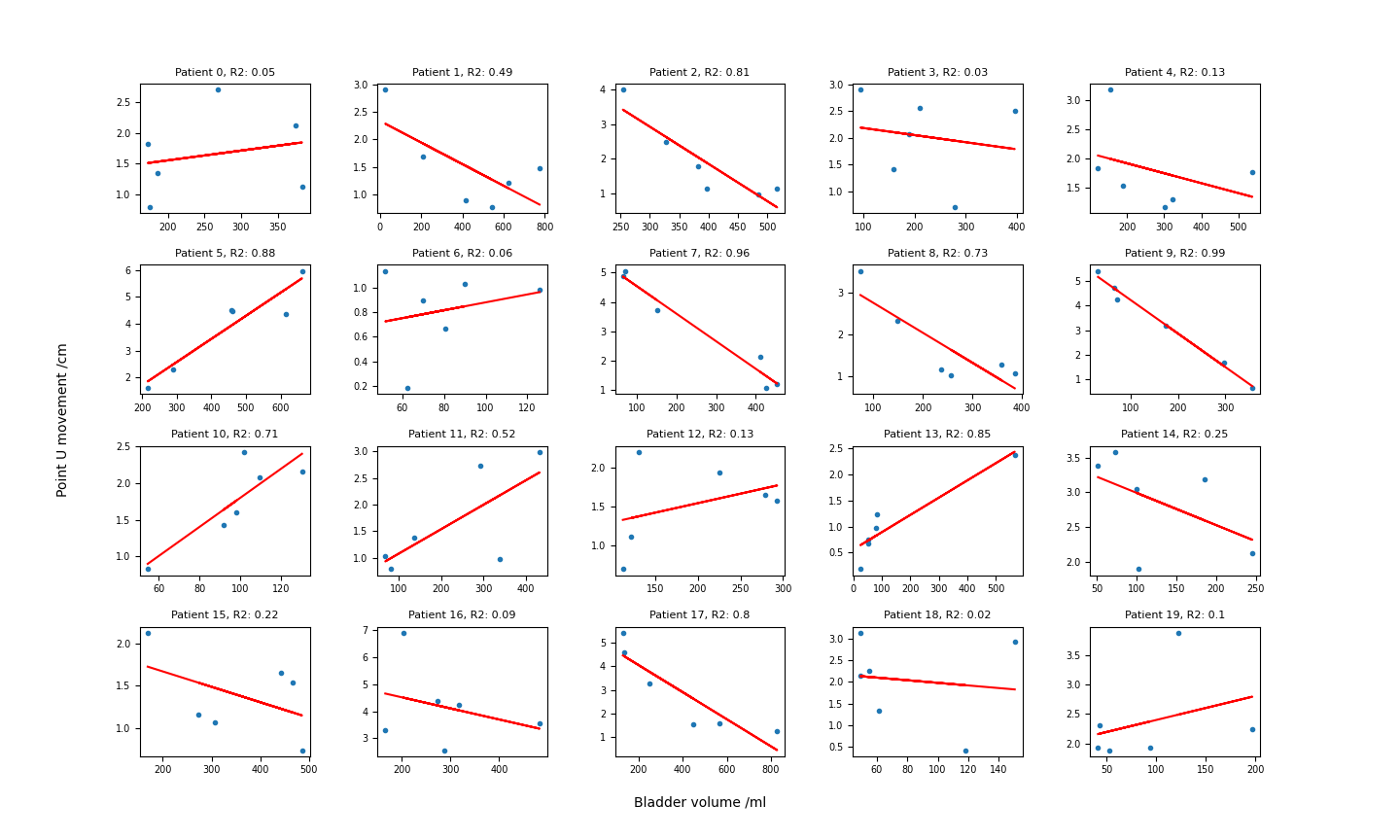
Variation was observed in bladder volumes (mean 239 ml, range 25-829), rectal diameters (mean 2.6 cm, range 1.1-5.7) and euclidean distance moved by U (mean 2.2, range 0.2-6.9), C (mean 1.3 cm, range 0.2-3.3), and CoM (mean 1.0 cm, range 0.1-3.1). For the overall cohort, bladder volume and rectal diameter did not correlate with distance moved by U, C or CoM (R2 all < 0.1). However, some individuals had stronger correlations; for U motion against bladder volume, 8 patients had R2 > 0.7 (Figure 1).
Patients with a stronger bladder-motion correlation had larger sigmoid volume on CT (p = 0.006) and more motion of CTVLR between full and empty-bladder CTs (more motion of the uterine fundus tip, p = 0.020; larger maximum surface-to-surface distance, p = 0.025; larger Hausdorff distance, p = 0.044). Details in Table 1.
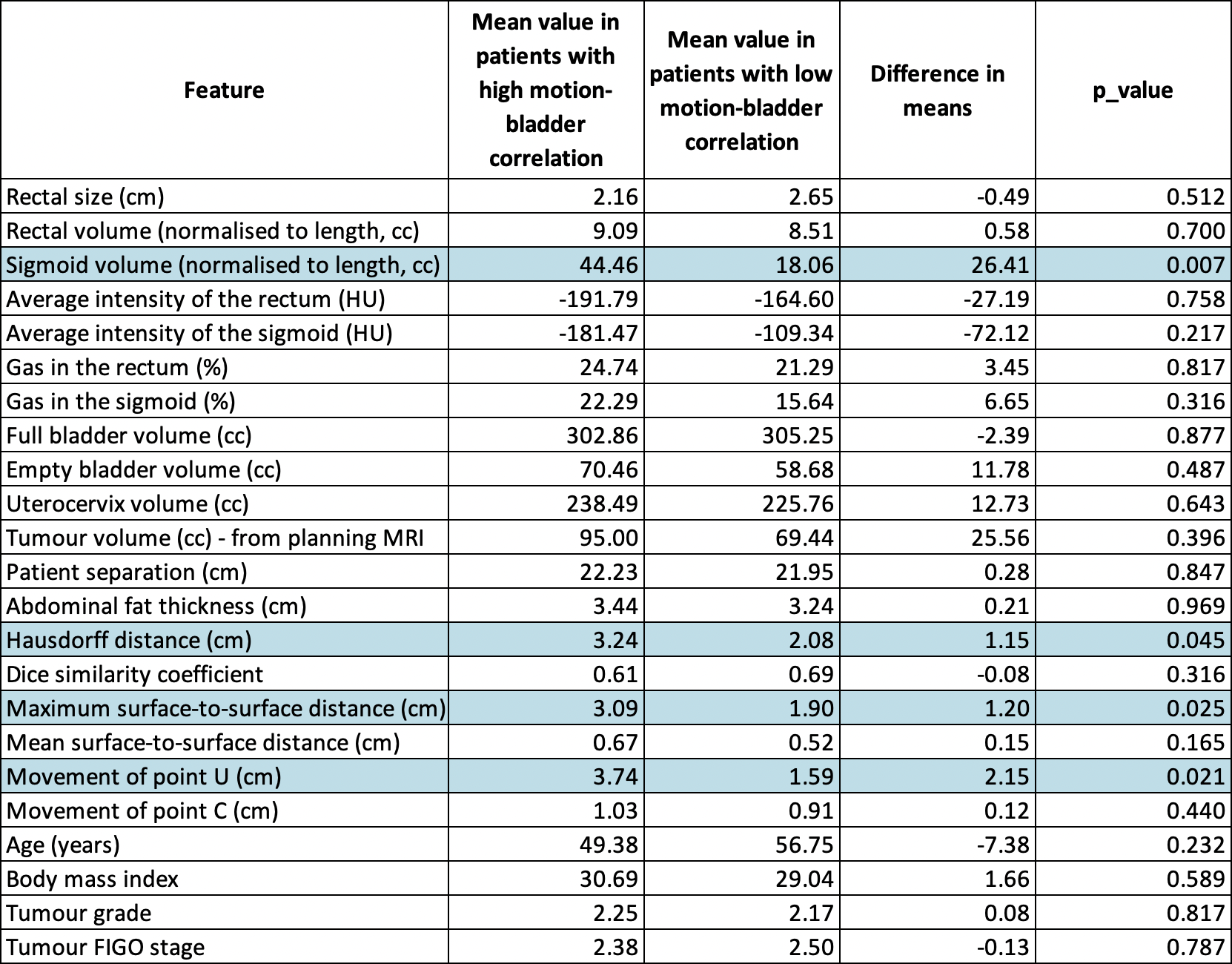
The slope of the relationship could be predicted pre-treatment based on sigmoid volume at planning, difference in bladder volume between full and empty CTs, tumour volume on MRI, and change in the superior extent of the CTVLR contour between full and empty planning CTs (linear regression, R2 0.77). Rectal size generally had weaker per-patient correlations with U, C and CoM. When bladder and rectal size were combined as explanatory variables, U motion could be predicted with confidence (R2 > 0.7) in 10 patients, C motion in 7 patients, and CoM motion in 8 patients.