Simulation of dose with reduction of tissue in breast radiotherapy
PO-1908
Abstract
Simulation of dose with reduction of tissue in breast radiotherapy
Authors: Mads Kjeldsen1, Martin Berg2, Henrik Nissen1, Else Maae1
1Vejle Hospital, Oncology, Vejle, Denmark; 2Vejle Hospital, Oncology, Vejle , Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
In breast radiotherapy (RT), the delivery of dose is planned from a ‘snapshot’ CT-scan. A major challenge is the changes in patient anatomy, mobility and positioning during treatment. Significant changes in tissue volume in the beam path are seen on daily cone-beam CTs and may result in unacceptable changes in the dose distribution. We have previously examined added tissue and are introducing a region of interest (ROI) in our clinic for daily CBCT evaluation of added tissue. The consequence of reduced tissue depth is less investigated. Decisions regarding missing tissue during treatment would benefit from a corresponding ROI, and should be equally considered to avoid risks of side effects in modern RT. Here we have undertaken a systematic dose calculation of tissue reduction, in order to clarify the treatments consequences.
Material and Methods
Twenty left-sided lumpectomy patients receiving 3D conformal RT were consecutively enrolled. All patients received irradiation to the breast and the loco-regional lymph nodes. Delineations were according to ESTRO guidelines. Treatment plans were made in Raystation 9 (RaySearch Laboratories AB, Sweden) according to the guidelines of the Danish Breast Cancer Group (DBCG) and local guidelines. During planning V105%=2% and V107%=2% was used as objective and constraint for the breast, respectively. For comparison, plans with other fractionations were converted to 40 Gy in 15 fractions by scaling the dose. Isotropic reduction of patient outer contours with 3, 4, 5, 7 and 10 mm reduction in turn was simulated, resulting in 6 scenarios including the original per patient. Target delineations were adjusted to maintain 5mm separation between CTVp_breast and simulated skin surface. Dose was recalculated using density override for each scenario and evaluated for 7 ROIs.
Results
The breast coverage, heart and lung dose is constant as shown in tabel 1. For the intermediastinal chain (CTVp_IC1-3) V90% increases, which is an improvement to the original dose. However, for the locoregional lymph nodes (CTVp_periclav) V90% decreases, and with a reduction of 5 mm or more the clinical effect of the treatment may be compromised. Hotspots increase for the breast CTV as shown in figure 1. The DBCG criteria V107% < 2% is exceeded when the reduction is 5 mm or more.
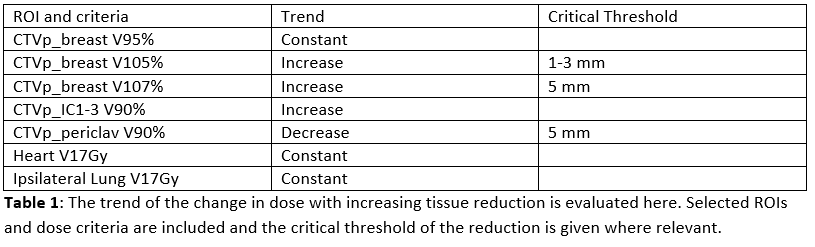
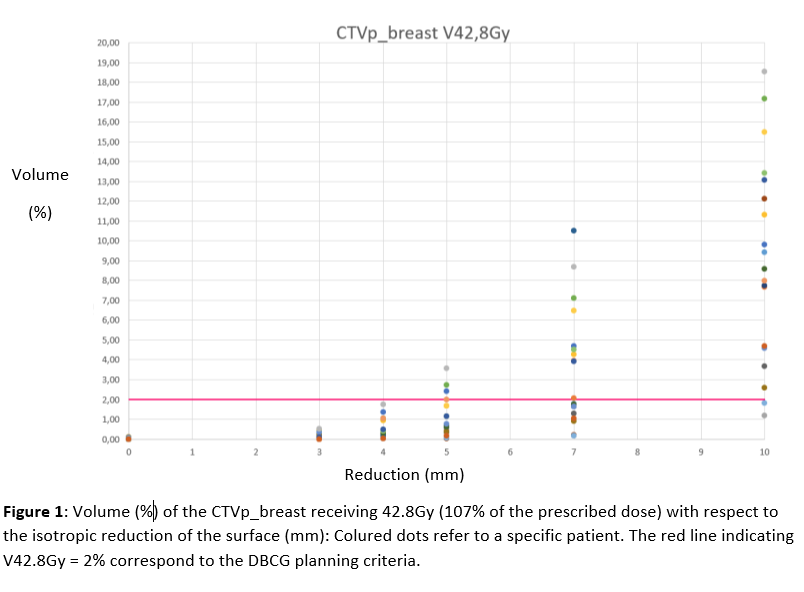
Conclusion
The impact of tissue reduction on the dose for breast RT shows that a reduction of 4mm or less results in an acceptable dose distribution for at full course when V105% < 2% is planned. For further tissue reduction V107% in the breast increase significantly and coverage of locoregional lymph nodes decrease significantly and thus adaption might be required taking the number of fractions, where the reduction occurs, into account. The dose to heart and ipsilateral lung is overall unchanged and acceptable even with major tissue reduction. The current study suggests a guidance ROI extending to 4 mm below the original skin surface with respect to tissue reduction.