Biomechanical imaging biomarker to predict tumor progression after head and neck chemoradiotherapy
PO-1695
Abstract
Biomechanical imaging biomarker to predict tumor progression after head and neck chemoradiotherapy
Authors: Koya Fujimoto1, Takehiro Shiinoki1, Yusuke Kawazoe1, Yuki Yuasa2, Wataru Mukaidani3, Yuki Manabe1, Miki Kajima1, Hidekazu Tanaka1
1Yamaguchi university, Department of radiation oncology, Graduate school of medicine, Ube city, Japan; 2Yamaguchi university hospital, Department of radiological technology, Ube city, Japan; 3Yamagucni university hospital, Department of radiological technology, Ube city, Japan
Show Affiliations
Hide Affiliations
Purpose or Objective
Biomechanical model (BM) based deformable image registration is a promising method for simulating morphological displacement of tumor and organs during radiotherapy (RT). Further, it is also reported as a beneficial imaging biomarker for organ function by capturing the mechanical behavior such as stress-strain relationship. The purposes are to construct the BM of the head and neck tumor to calculate stress changes during the RT using the longitudinal computed tomography (CT) and to evaluate its predictive performance of the tumor progression after the head and neck chemoradiotherapy.
Material and Methods
This study included 53 patients with stage Ⅱ-Ⅳ squamous cell carcinoma (SCC) of the nasopharynx, oropharynx and hypopharynx who had been treated with definitive chemoradiotherapy via volumetric modulated arc therapy with a total dose of 70 Gy in 35 fractions between 2015 and 2019. All patients underwent treatment planning CT one week before (pre-RT) and three weeks after the start of RT (mid-RT). Figure.1 shows the workflow of this study. For both pre-RT and mid-RT CT images, the tumor structures were delineated by a radiation oncologist and those were meshed in 2.0 mm. The boundary conditions of tumor BM were optimized as the dice metrics and mean distance to agreement between deformed pre- and mid-RT tumor structure were at least 0.90 and within 1.0 mm, respectively. The retrospective univariate analysis with a Mann-Whitney U test were conducted which correlated tumor progression occurring within 2 years after RT with the patient characteristics. The characteristics included in the analysis were as follows: biomechanics driven tumor stress (TS) and tumor volume reduction rate (TVRR) between pre-RT with mid-RT, pre-RT-tumor volume (pre-RT-TV), age, sex, smoking, tumor staging (T stage, N stage and TNM stage), tumor site and presence of concurrent chemotherapy. Moreover, for each tumor TNM stage, the TS and TVRR in the group with and without tumor progression were compared.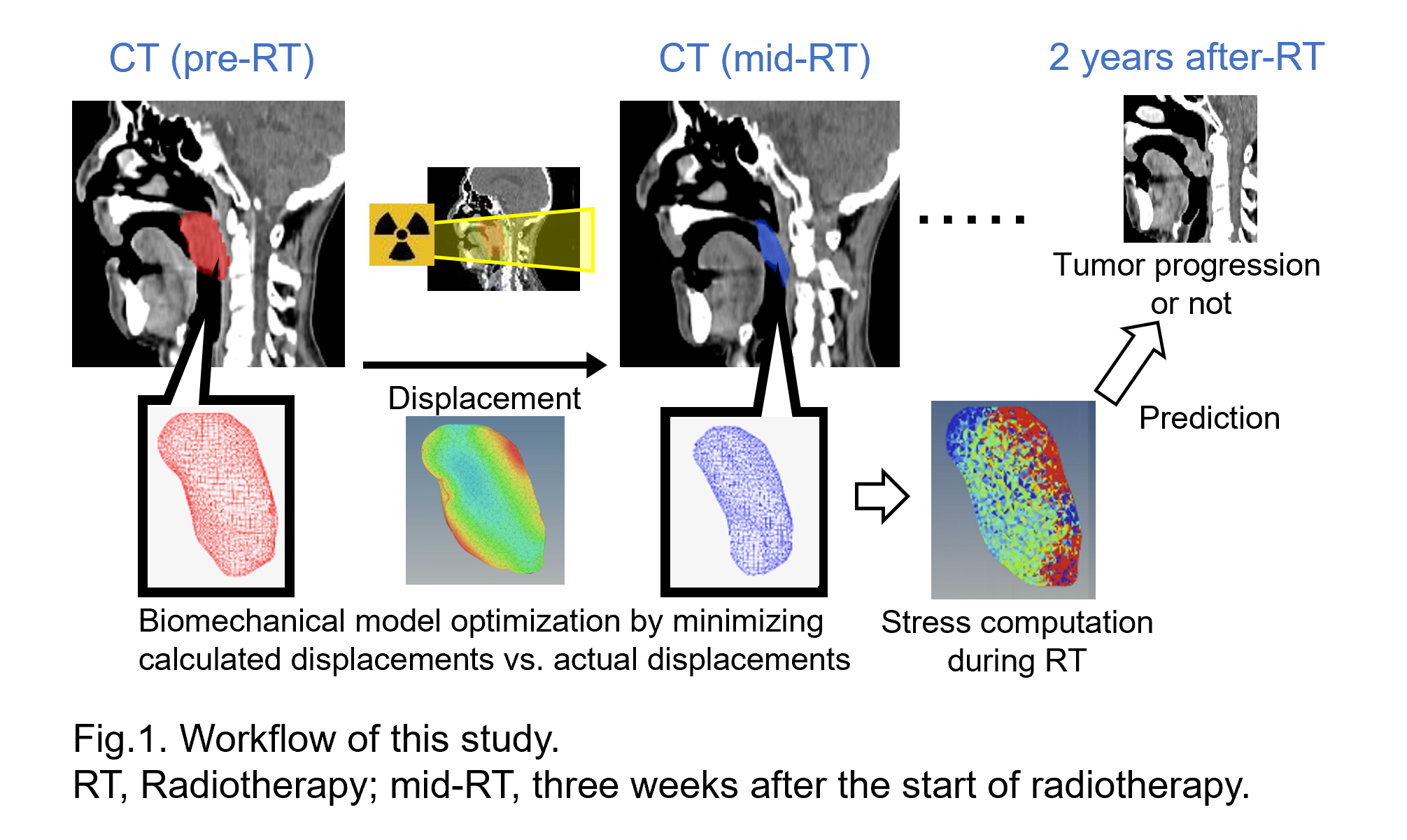
Results
Figure 2 shows the summary of results. On univariate analysis, TS, TVRR and pre-RT-TV were identified as a significant predictor of tumor progression occurring within 2 years after RT (Fig.2 (a)). The critical cutoff point for the TS was identified as 650 Pa with the area under the receiver operating characteristic curve (AUC) of 0.86. Furthermore, for both TNM stage of Ⅱ-Ⅲ and Ⅳ, there were significant difference in TS between the group with and without tumor progression occurring within 2 years after RT (p<0.01), but not in TVRR (Fig.2 (b)) .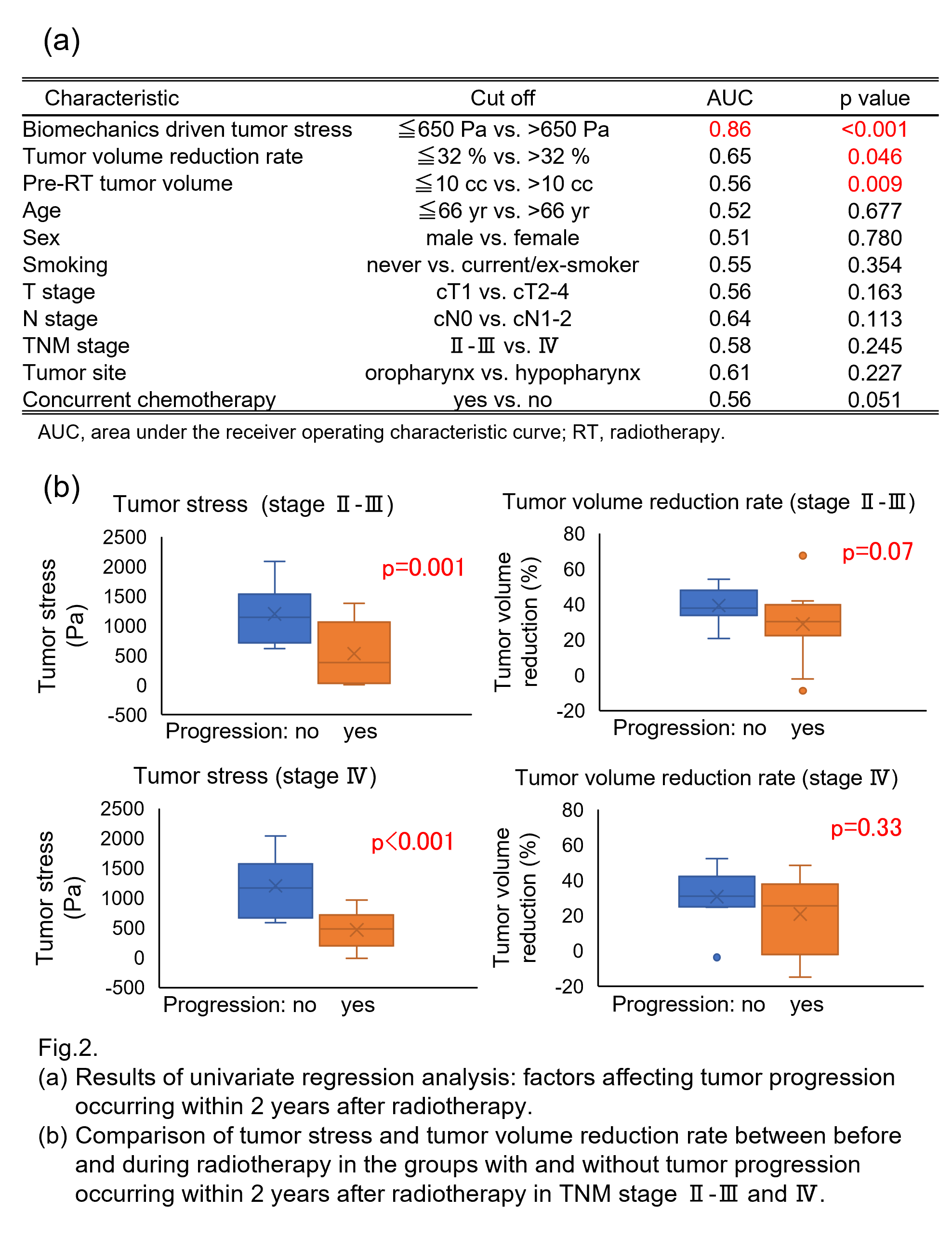
Conclusion
The results of our study have shown that the tumor stress derived from BM with the longitudinal CT between pre-RT and mid-RT is a significant prognostic factor in patients with head and neck SCC underwent definitive chemoradiotherapy and correlated with the tumor progression better than the patient characteristics such as tumor staging, and TVRR.