Accuracy of dose calculation using a novel high-performance cone-beam CT imager
PO-1683
Abstract
Accuracy of dose calculation using a novel high-performance cone-beam CT imager
Authors: Marta Bogowicz1, Vicki Trier Taasti1, Gabriel Fonseca1, Didier Lustermans1, Colien Hazelaar1, Hendrik Hansen1, Femke Vaassen1, Richard Canters1, Wouter van Elmpt1
1Department of Radiation Oncology (MAASTRO), GROW – School for Oncology and Reproduction, Maastricht University Medical Centre+, Maastricht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Cone-beam CT (CBCT) imaging has always been hampered by lower image quality than fan-beam CT. Furthermore, dose calculation based on CBCT scans has been less precise. In this work we evaluated the dose calculation accuracy for a novel CBCT system integrated in a standard linear accelerator.
Material and Methods
A pre-clinical release of a high-performance CBCT imager (HyperSight™) integrated in a Halcyon (v4.0, Varian Medical Systems) treatment machine was evaluated for dose calculation purpose. This system incorporates a high-power kV source combined with a novel large flat panel detector (86x43 cm2) and software for CBCT iterative reconstruction with advanced scatter corrections (Acuros® CTS and Monte-Carlo based hardware scatter model) and metal artifact reduction (MAR). A CBCT-to-mass density calibration was performed (Gammex Advanced Electron Density Phantom, Sun Nuclear).
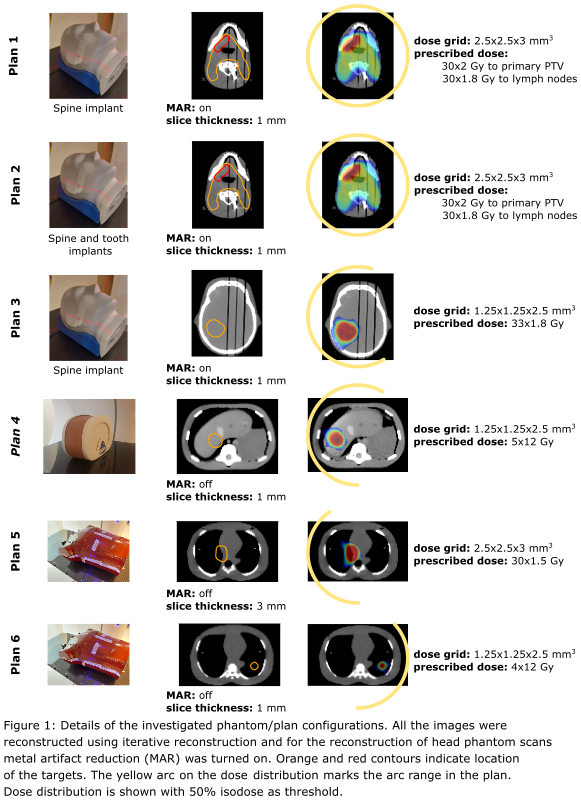
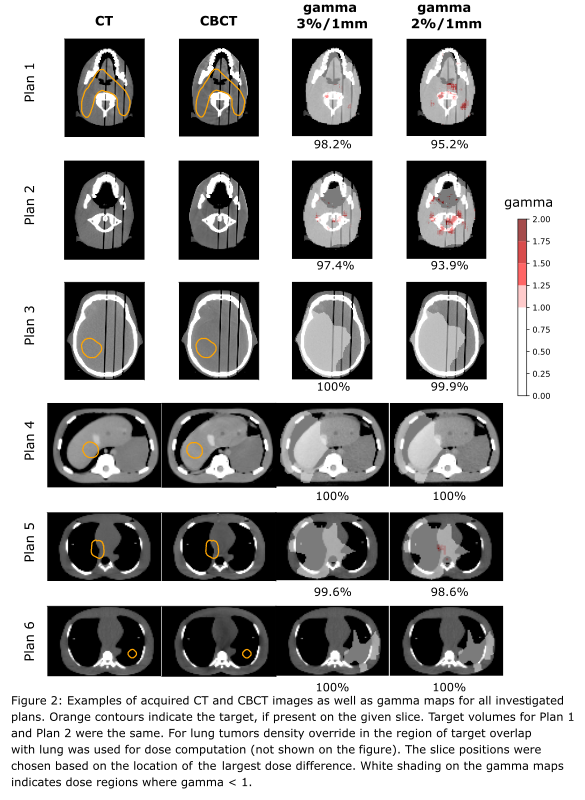
For a comprehensive dose comparison, phantoms for 3 different body sites were used: head-and-neck (CIRS Proton Therapy Dosimetry Head, Sun Nuclear), thorax (Alderson RANDO, RSD Radiology Support Devices) and abdomen (CIRS Triple Modality 3D Abdominal Phantom, Sun Nuclear). In total 6 plans were created (Fig. 1). The plans encompassed a wide range of target locations and plan complexities. Targets and organs-at-risk (OARs) were defined on the planning CT images (SOMATOM Confidence, Siemens). Treatment plans were optimized and calculated in Eclipse™ (Acuros v17). CT and CBCT scans were rigidly registered, contours were copied and plans were re-calculated with fixed monitor units on the CBCT scan. Differences in Dmean to relevant target volumes and OARs were evaluated and gamma analysis was performed (3%/1 mm and 2%/1 mm, dose normalized to prescription dose, 20% dose threshold).
Results
Good agreement was found between the doses calculated on CT and re-calculated on CBCT scans. For all phantoms mean PTV dose difference was below 0.5 Gy, with CBCT-based calculation resulting in slightly higher doses. Small dose differences were also observed in Dmean to surrounding OARs. Dose difference was below 0.5 Gy for all OARs analyzed for Plans 1, 3, 5 and 6. In the CBCT-based dose re-calculation for Plan 2 (configuration with multiple metal implants), the Dmean to the left parotid was underestimated by 0.6 Gy and the Dmean to the middle pharyngeal constrictor muscle was overestimated by 0.8 Gy. For Plan 4, the Dmean to a 0.5 cm ring around the PTV was underestimated by 0.6 Gy. All plans had excellent gamma agreement, 3%/1mm > 97%, and only Plan 2 had gamma agreement 2%/1mm < 94% (Fig. 2).
Conclusion
We characterized the dose calculation accuracy for a novel CBCT imager. Very good agreement between dose calculations performed on the CBCT and planning CT was observed. MAR reconstruction provided good dose accuracy when a large implant was placed close to the target. This novel CBCT system with enhanced image quality and CT number accuracy opens a large variety of possibilities for direct off-line and online re-planning.