The Dosimetric Implications of Sentinel Node Mapping on Adjuvant Radiotherapy for Endometrial Cancer
Thomas Charlton,
United Kingdom
PO-1436
Abstract
The Dosimetric Implications of Sentinel Node Mapping on Adjuvant Radiotherapy for Endometrial Cancer
Authors: Thomas Charlton1, Angharad Ganguli2, Nana Gomes3, Katherine Mackay4, Alexandra Taylor5
1The Royal Marsden NHS Foundation Trust , Clinical Oncology , London, United Kingdom; 2The Royal Marsden NHS Foundation Trust , Radiotherapy, London , United Kingdom; 3The Royal Marsden NHS Foundation Trust , Surgery , London , United Kingdom; 4The Royal Marsden NHS Foundation Trust, Clinical Oncology, London, United Kingdom; 5The Royal Marsden NHS Foundation Trust, Clinical Oncology, London , United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Most patients with endometrial cancer present early and are treated with surgery. Adjuvant therapy is determined according to recent ESGO-ESTRO-ESP guidelines (1). Those in the High-intermediate and High-risk groups are offered a combination of radiotherapy (EBRT), vaginal vault brachytherapy (VVB), with or without chemotherapy.
Sentinel Lymph Node (SLN) mapping is increasingly used to determine which patients may benefit from adjuvant EBRT.
SLNs may be located beyond the pelvis and in those with involved pelvic nodes, 51% may also have involved para-aortic (PA) nodes (2). Traditional EBRT target volumes with a superior border of L5/S1 may not provide adequate coverage.
This study maps SNL location and considers the dosimetric impact of extending target volumes to include the common iliac and PA regions.
Material and Methods
39 patients who received EBRT with or without VVB between January 2020 and February 2022 were included. Pre-operative imaging and SLN biopsies were used to map the location of primary station and involved lymph nodes.
10 consecutive patients who were scanned to a superior extent of T12 were identified. Target volumes were contoured to include the traditional pelvic volume (CTV A), extended to include the pre-sacral and common iliac region (CTV B) and the PA region (CTV C). A 5mm margin was added to create PTV A-C respectively.
These were planned with VMAT to receive a prophylactic dose of 45 Gy in 25 fractions. Clinical dose constraints included rectum (V30 Gy<80%), bowel (V45 Gy<139 cm3), kidney (mean dose <15 Gy), duodenum (V55 Gy<15cm3) and spinal cord (Dmax <50 Gy).
Results
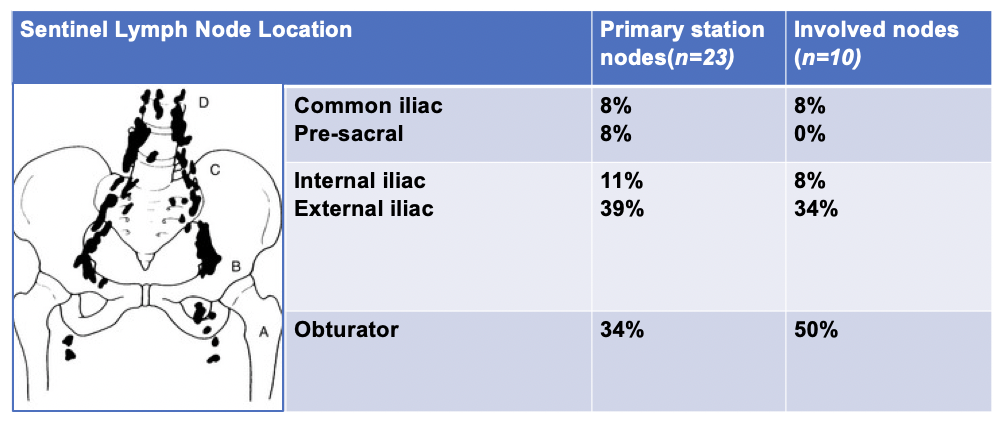
The primary station lymph node was recorded in 23/39 patients (59%). Most primary station nodes (84%) were in the pelvis, with 16% located beyond in the pre-sacral and common iliac regions (Figure 1).
The involved lymph node detection rate was 8% on pre-operative imaging versus 28% of SLN mapping.
In the dosimetric study, extending the radiotherapy target volumes from PTV A-C met the PTV and OAR constraints used in clinical practice.
Conclusion
SLN mapping improved involved node detection from 8% to 28%. Most primary station nodes were in the pelvis, however, 16% were found beyond traditional EBRT target volumes in the pre-sacral and common iliac regions. From a dosimetric perspective, extending target volumes to include these areas met clinical dose constraints.
Whilst further work is required to understand the therapeutic benefits and associated toxicities in clinical practice, extended target volumes have the potential to reduce the risk of nodal recurrence for this patient group.
1) Concin N et al. ESGO/ESTRO/ESP guidelines for the management of patients with endometrial carcinoma. International Journal of Gynecologic Cancer. 2021 Jan 1;31(1).
2) Kumar S et al. Prospective assessment of the prevalence of pelvic, paraaortic and high paraaortic lymph node metastasis in endometrial cancer. Gynecologic oncology. 2014 Jan 1;132(1):38-43.