Impact of radiation on immune cells in patients with low-grade brain tumor
Yoo Kyung Choi,
Korea Republic of
PO-1156
Abstract
Impact of radiation on immune cells in patients with low-grade brain tumor
Authors: Yoo Kyung Choi1, Jin Ho Song2
1Seoul Saint Mary's Hospital, Radiation Oncology, Seoul, Korea Republic of; 2Seoul Saint Mary's Hospital, Radiation Oncology, Seoul, Korea Republic of
Show Affiliations
Hide Affiliations
Purpose or Objective
The proportion of circulating immune cells may play an essential role in the treatment of patients with brain tumors. Numerous studies to demonstrate the effects of radiation therapy on hematological variables have been conducted mostly for high-grade glioma patients receiving concurrent radiotherapy with chemotherapy or steroids. In this study, we focused on low-grade brain tumors to rule out the impacts of chemotherapy and steroid use. The change of NLR, neutrophil counts, and lymphocytes counts were evaluated in order to find significant factors influencing those changes. We examined the effects of radiation therapy on circulating immune cells and identified significant factors in order to reduce possible RT-induced immunotoxicity.
Material and Methods
Patients with low-grade brain tumors who were diagnosed as WHO grade I or II and received brain RT between 2007 and 2020 were included. A total of 46 patients were eligible and included. The primary endpoint was the critical factors for the change of NLR, neutrophil counts, and lymphocyte counts before and after the treatment. The secondary endpoint was the difference of the changes of NLR, neutrophil counts, and lymphocyte counts between the 3D-CRT and the IMRT group.
Results
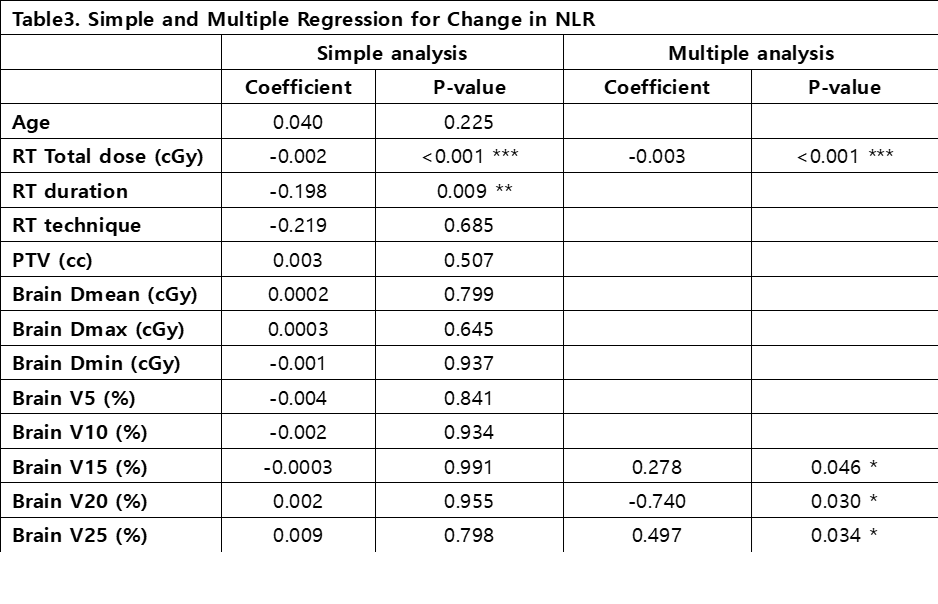
Regarding the change in NLR, the radiation total dose significantly lowered NLR value both in simple and multiple regression. The total duration of radiation treatment significantly lowered NLR value in a simple analysis. PTV , however, was not correlated with the change of NLR values. In a multiple regression, RT total dose, Brain V15, Brain V20, and Brain V25 were significant factors in changing NLR values. However, there was no difference in the changes of NLR values between IMRT and 3D-CRT techniques.
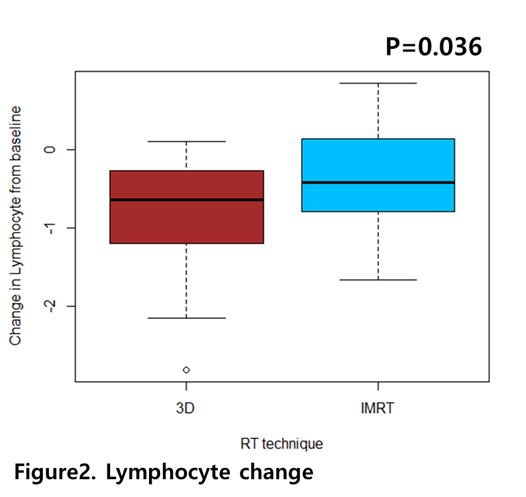
The change of ALC was significantly correlated with RT technique in a simple regression. In a multiple regression, PTV, Brain V5 and Brain V15 were selected variables. PTV was marginally related (p=0.059), and Brain V5 and Brain V15 were statistically significant (p=0.029, p=0.005, respectively). ALC more decreased in 3D-CRT group than in IMRT group after treatment.
In a simple regression, there were no significant variables related to the change of ANC. However, stepwise regression selected age, RT duration, PTV, Brain V10, and Brain V20 as critical variables. PTV and Brain V20 were significantly related to the change of ANC. PTV marginally explained the change of ANC. The mean of the change of ANC was similar between IMRT group and 3D-CRT group.
Conclusion
IMRT effectively lowered the risk of decrease in ALC compared to 3D-CRT. We may be able to prevent RT-induced lymphopenia by lowering Brain V15, which is a significant predictor of ALC. In addition, shrinking PTV as much as possible might be beneficial for preventing neutrophilia. Taken together, our findings support that using IMRT and modifying dosimetric dose may achieve the declined NLR that is associated with a favorable prognosis.