Transitioning from conventional photon therapy to proton therapy for primary brain tumors
Per Munck af Rosenschold,
Sweden
PO-1148
Abstract
Transitioning from conventional photon therapy to proton therapy for primary brain tumors
Authors: Per Munck af Rosenschold1, Hanna Ek2, Ingrid Fagerström Kristensen2, Lars Stenberg3, Sara Kinhult2, Hunor Benedek1, Simon Ek4, Svend Aage Engelholm5, Silke Engelholm2
1Lund University and Skåne University Hospital, Hematology, Oncology and Radiation Physics, Lund, Sweden; 2Skåne University Hospital, Hematology, Oncology and Radiation Physics, Lund, Sweden; 3Skåne University Hospital, Radiology, Lund, Sweden; 4Lund University, Physics, Lund, Sweden; 5Rigshospitalet, Oncology, Copenhagen, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Proton radiation therapy (PT) is increasingly selected over photon radiotherapy (XRT) in treatment of low-grade gliomas patients (LGG), due to superior radiation dose-sparing of brain tissue. In this single-institution retrospective study we investigate the influence on treatment planning practices and treatment outcomes, including pseudo-progression (PsP) and survival, for LGG by the introduction of PT.
Material and Methods
Adult patients with grade 2-3 glioma consequtively treated with PT or XRT from May 2012 to December 2019 were included. Tumor characteristics and treatment data were collected. The groups treated with PT and XRT were compared regarding treatment characteristics, side effects, occurrence of PsP and survival outcomes.
Results
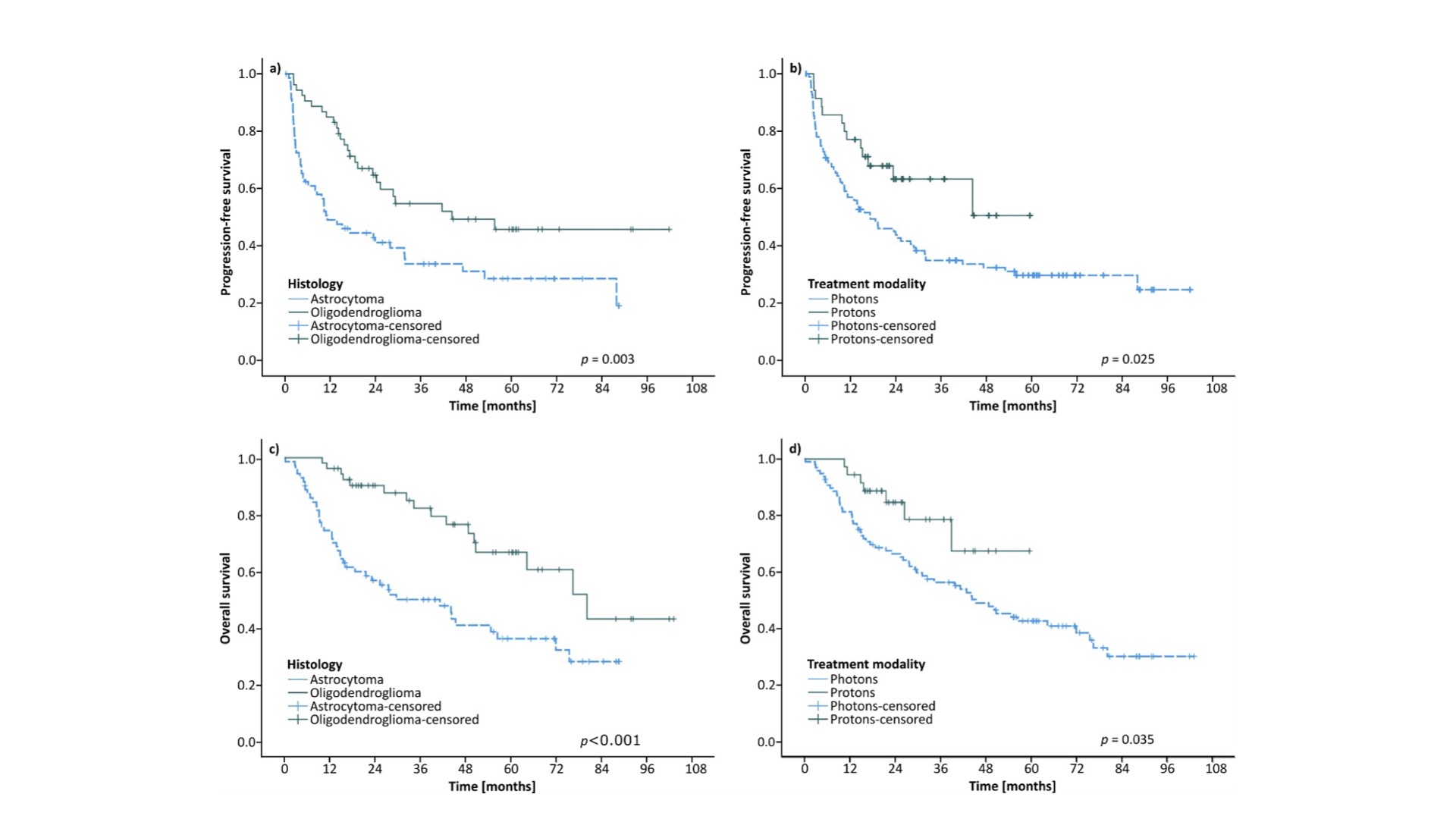
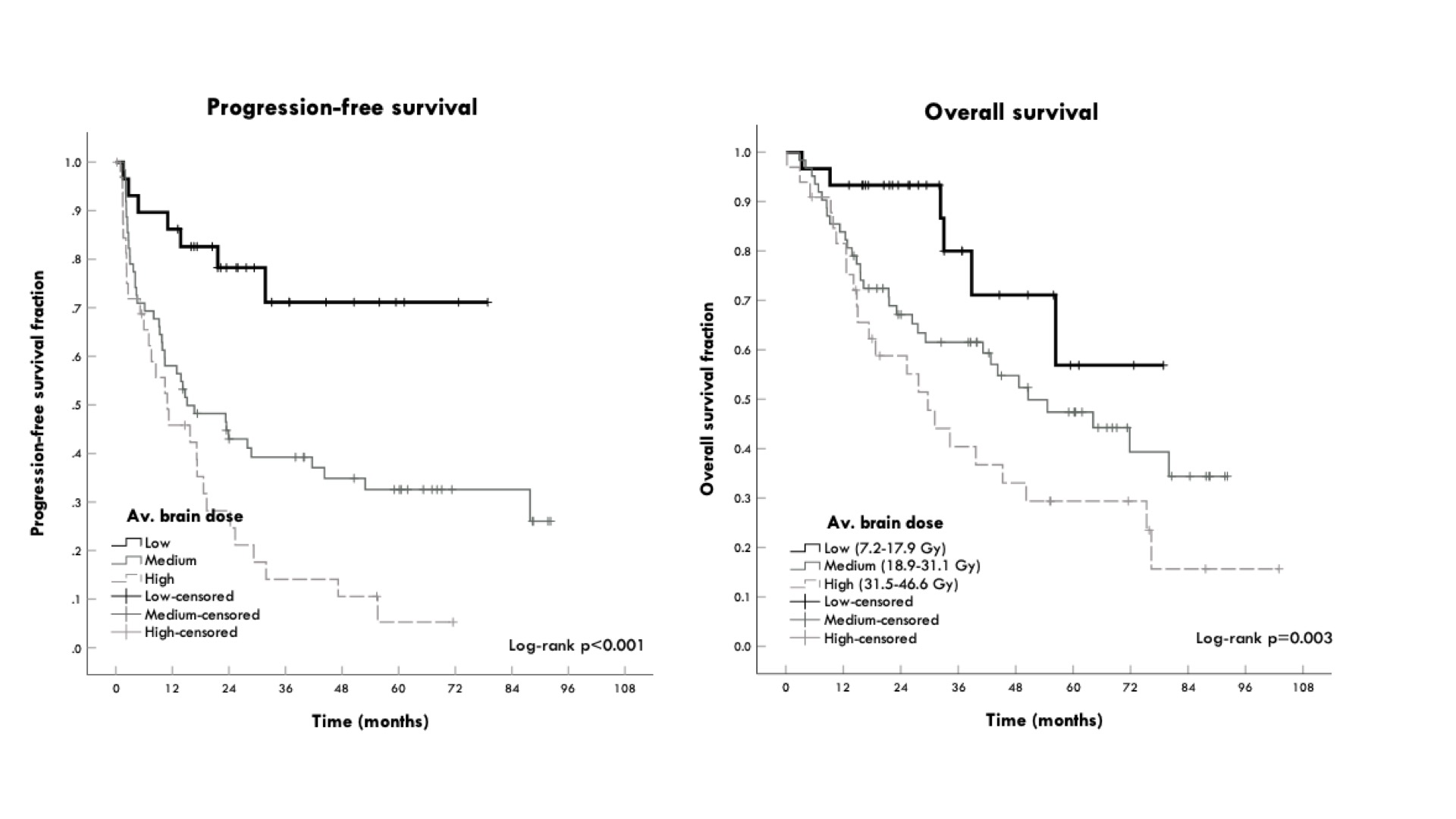
Out of 143 patients meeting the inclusion criteria, 44 were treated with PT, 98 with XRT and one with mixed PT+XRT. The patients receiving PT were younger, had a lower tumor grade, more often oligodendrogliomas and received a lower mean brain and brainstem dose. PsP was observed in 21 out of 126 patients, with no difference between XRT and PT (p=0.38). The rate of fatigue in immediate connection to RT (<3 months after) was higher for XRT than for PT (p=0.016). The PT patients had a significantly better PFS and OS than the XRT patients (p=0.025 and 0.035). Progression-free survival and overall survival data are shown in Figure 1. Higher average dose to both brain and brainstem was associated with inferior PFS and OS (p<0.001). By way of splitting the cohort in 3 groups based on their average brain dose; low dose (bottom 25% percentile), medium (25-75% percentile) and high dose (top 25% percentile), it is apparent that both the progression-free survival is dramatically impacted. Potentially, either average dose to the brain (or dose to the brainstem) might be suited for prognostication as compared to other clinical prognostic factors.
Conclusion
The superior PFS and OS outcomes for PT indicates that the tumor and characteristic-based treatment modality selection process is beneficial for the patients, though average brain dose may be better suited for this purpose. There was no difference in PsP for XRT and PT. PT was associated with lower rates of fatigue <3 months after RT.