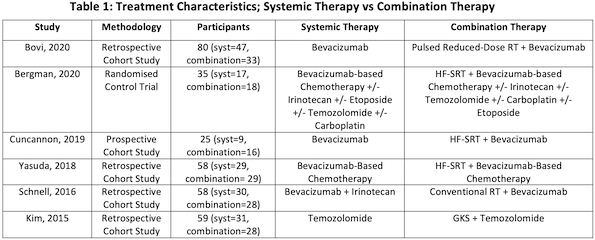
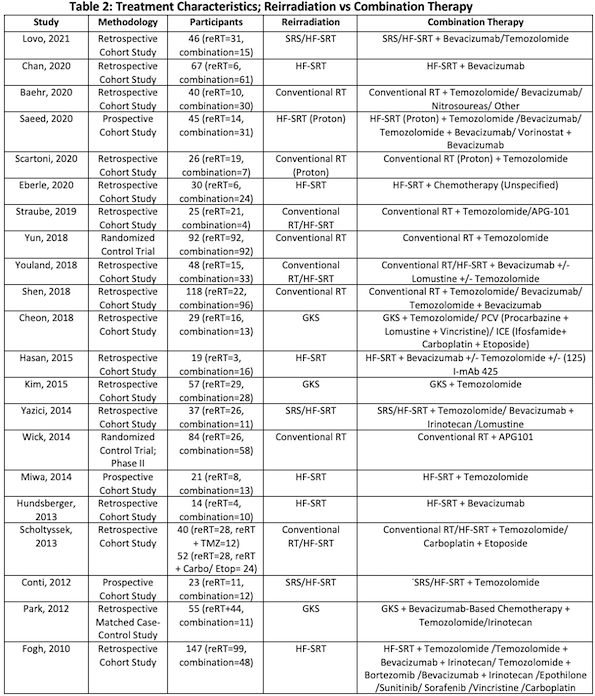
28 studies were included. In the systemic therapy vs reirradiation group; there was no difference in OS (3 studies, 237 participants; HR 0.83 (95%CI 0.51-1.35), p=0.45, I2=37%) and PFS (2 studies, 185 participants; HR 0.80 (95%CI 0.55-1.18), p=0.26, I2=0%). In the systemic therapy vs combination therapy group (Table 1); combination therapy improved OS (5 studies, 290 participants; HR 0.59 (95%CI 0.44-0.77), p=0.0002, I2=0%) and PFS (4 studies, 232 participants; HR= 0.53 (95%CI 0.36-0.77), p=0.001, I2=44%), and there was no difference in grade 3+ AEs (3 studies, 151 participants; RR 1.32 (95%CI 0.58-3.01), p=0.50, I2=0%). In the reirradiation vs combination therapy group (Table 2); combination therapy improved OS (14 studies, 805 participants; HR 0.60 (0.48-0.75), p<0.0001, I2=29%) and PFS (5 studies, 259 participants; HR 0.48 (95%CI 0.35-0.65), p<0.00001, I2=0%), and combining reirradiation with bevacizumab reduced radionecrosis (3 studies, 129 participants; RR 0.04 (95%CI 0.01-0.23, p=0.0002, I2=0%). Subgroup analysis of studies accounting for confounders through methodology or multivariate analysis reaffirmed these results. A meta-analysis could not be conducted on QoL outcomes due to insufficient reporting.