Radiation necrosis in patients treated with brain SRT: evaluation of clinical and dosimetric factors
PO-1120
Abstract
Radiation necrosis in patients treated with brain SRT: evaluation of clinical and dosimetric factors
Authors: Angela Barillaro1, Mara Caroprese2, Caterina Oliviero3, Stefania Clemente3, Christina Amanda Goodyear4, Antonio Russo4, Laura Cella5, Roberto Pacelli6, Manuel Conson7
1Federico II University School of Medicine, Department of Advanced Biomedical Sciences, Naples, Italy; 2Federico II University School of Medicine, Department of Advanced Biomedical Sciences, Naples, Italy, Italy; 3Federico II School of Medicine, University Hospital, Naples, Italy; 4Federico II School of Medicine, Department of Advanced Biomedical Sciences, Naples, Italy; 5Institute of Biostructures and Bioimaging, National Research Council of Italy (CNR), Naples, Italy; 6University of Naples Federico II, Department of Advanced Biomedical Sciences, Naples, Italy; 7University of Naples Federico II, Department of Advanced Biomedical Sciences,, Naples, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
SRT is a proven effective treatment for brain metastases (BM), but radiation necrosis (RN) is a possible late effect affecting patient's QoL. We report the outcome and the incidence of RN in patients treated at a single institution.
Material and Methods
44 patients treated for treated for 116 BM with SRT from 2016 to 2021 with clinical and MRI follow up ≥6 months were selected. Survival outcomes were estimated with the Kaplan-Meier method. RN was scored according to the CTCAE 5.0. Clinical (KPS, histology, extracranial disease status, smoking status, chemo-, immuno- or target-therapy, steroids use during RT, previous brain treatments), anatomical (PTV volume, location) and dosimetric (BED2 corrected brain minus GTV Dmax and Vx across 2 Gy increments of dose) factors were collected. To evaluate factors possibly associated with RN, univariate and multivariate logistic regression analyses. ROC analysis was also performed.
Results
At a median follow up of 16 (6-42) months the crude local control is 90%. Estimated median OS, extracranial-PFS, brain-PFS are 25, 9 and 11 months, respectively. Estimated LFFS rates at 1-, 2- and 3-years result 89.7%, 85.3% and 85.3%, respectively; extracranial-PFS 36.7%, 23.8%, and 15.9%; brain-PFS 37.9%, 21.4%, 10.7%. OS is significantly better when KPS is ≥70 (p=.004) (Figure 1). G1-2 RN occurred in 11 patients (25%) and 16 lesions (14%), with a median time to onset of 6 (3-46) months. G2 patients with neurological deficits received steroids, and 40% improved or stabilized with treatment, although for all of them a phase of 5-16 months of steroids dependence has been faced (Figure 2); for others, the event is still ongoing (20%), or not evaluable (40%). No one required surgical decompression (G3). At univariate analysis, previous surgery (p=.02), PTV (p=.006) and GTV (p=.003) size resulted significantly related to RN. Dosimetric parameters resulted not significantly related with RN. Median PTV size was 1.21(0.02-25.2) cc for the G0 RN, and 2.72(0.75-89.38) cc for the G1-2, respectively. A cut-off value of 1.48 cc for the PTV size was found by ROC analysis. G1-2 events occurred in the 26% of BM with PTV ≥ 1.48 cc. Incidence of RN was 100% for surgery BM, which is the only factor remained significant at multivariate analysis.
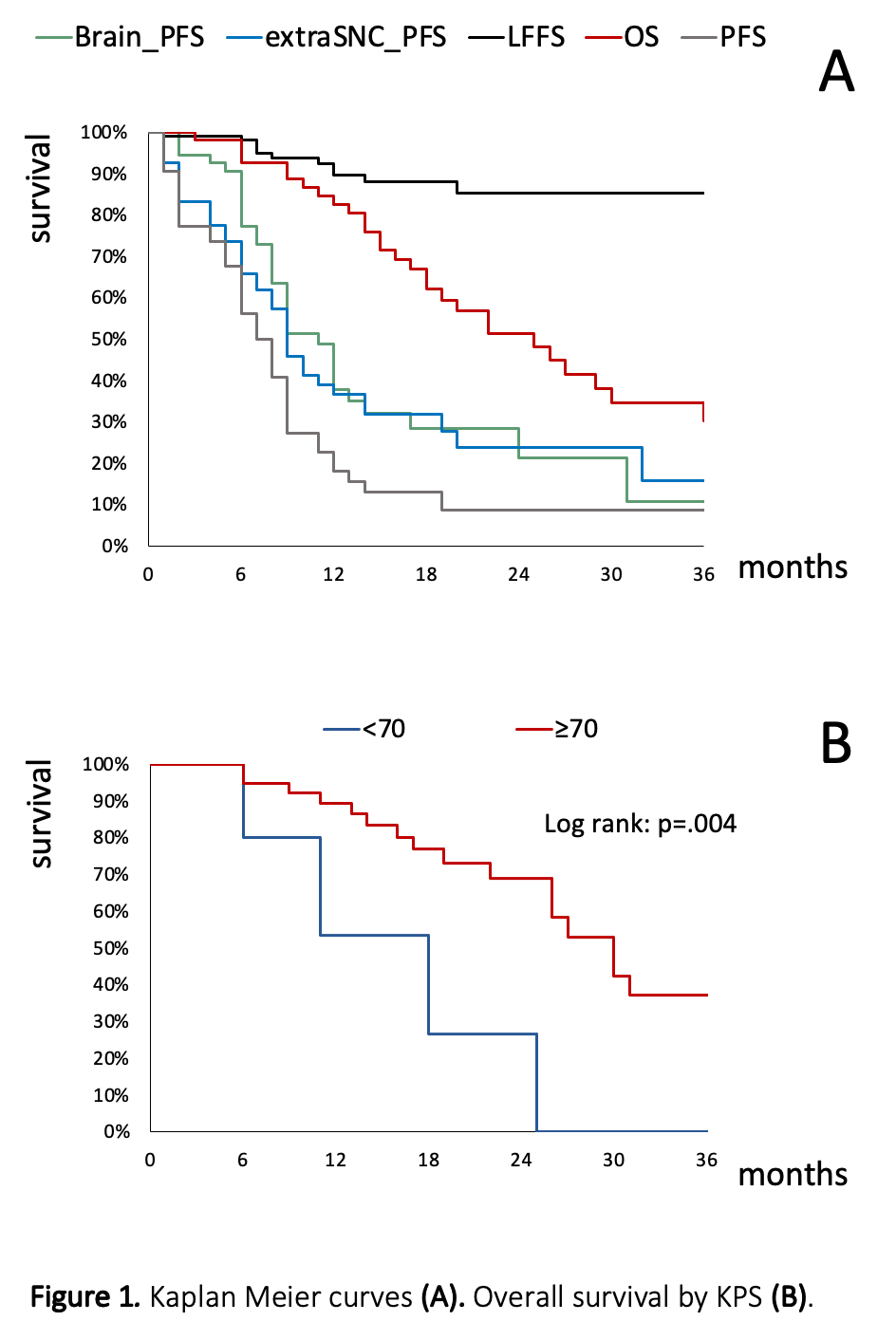
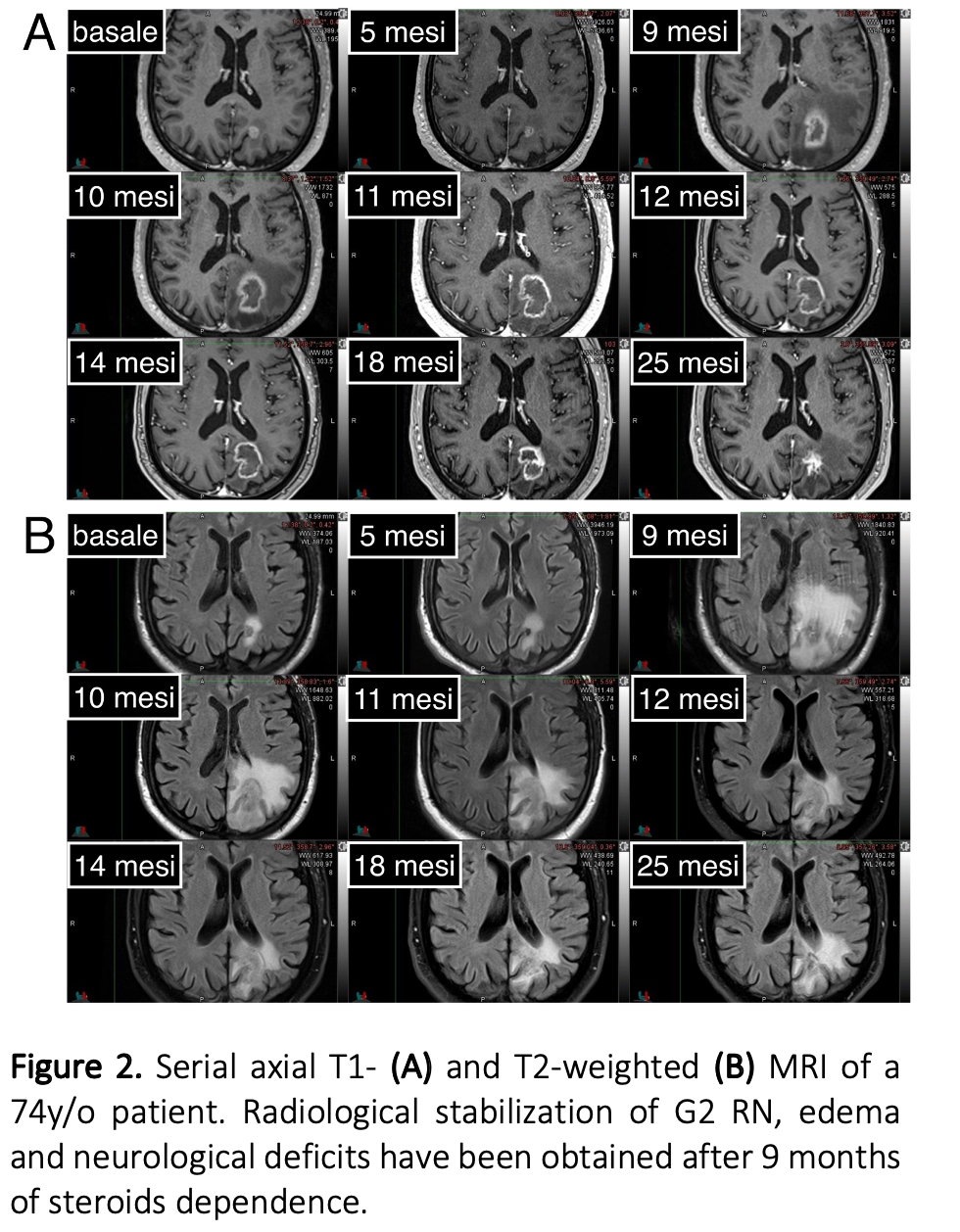
Conclusion
SRT, regardless of primary histology, is an effective treatment for BM with survival mostly depending on KPS. The observed incidence of RN was consistent with that reported in the literature. RN diagnosis and treatment remain challenging, but in our experience, with prompt recognition and medical therapy, radiological and clinical stabilization was obtained in most cases. However, further FUP is warranted. Risk-benefit ratio evaluation and particular radiological/clinical attention could be required when PTV>1.48cc.