Brain directed therapy followed by systemic treatment in metastatic renal cell carcinoma
Maha Zarroug ,
United Kingdom
PO-1118
Abstract
Brain directed therapy followed by systemic treatment in metastatic renal cell carcinoma
Authors: Maha Zarroug1, Ahmed Shaheen1, Ahmed Mohammed1, Manal Elgendy1, Alexander Burns1, Mohammed AlHilali1, Marieke Vanderputten1, Ashraf Azzabi1, Robert Chandler1, John Frew1, Hannah Hayhurst1, Malcolm Jackson1, Ian Pedley1, Rachel Pearson1, Xue-Yan Jiang1
1The Newcastle upon Tyne NHS Foundation Trust, Northern Centre for Cancer Care, Newcastle upon Tyne, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
To assess the impact of brain directed therapy (BDT) in patients with metastatic renal cell carcinoma (mRCC) with brain metastases (BM), who have received stereotactic radiosurgery (SRS) – with or without surgery, and systemic anti-cancer therapy (SACT) in the Northern Centre for Cancer Care (NCCC), United Kingdom (UK).
Material and Methods
This is a retrospective analysis of patients diagnosed with mRCC between January 2018 and July 2022 who then developed brain metastases and received brain directed therapy. Data was extracted from the chemotherapy register and cross referenced with the radiotherapy database and medical electronic records in the NCCC, UK.
Results
We identified n=28 patients (16.2 %) out of 172 who had developed brain metastases during the period. IMDC favourable, intermediate, and poor risks distribution were 9, 13, 6 respectively. Median age was 65 (54 – 77). 19 (67.8%) patients were male and 9 (38.3%) were female. Twenty-six (15.1%) were symptomatic, and 2 (1.1%) were asymptomatic. 10 (35.7%) were SACT naïve, 10 (35.7%) were on first line treatment with tyrosine kinase inhibitor (TKI), 1 (3.6%) were on first line immunotherapy (IO) and 7 (25.0%) had multiple lines of treatment including TKI and IO.
Twenty (71.4%) patients received BDT (16 (57.1%) received radiotherapy, 2 (7.1%) received SACT alone and 2 (7.1%) had surgery alone). Eight (28.5%) were placed on best supportive care (BSC) with no further SACT.
Of the 16 patients (57.1 %) who received radiotherapy, 3 (10%) received whole brain radiotherapy (WBRT), 13 (6.0%) received SRS using VMAT technique, with doses ranging between 15 and 25 Gy in 1 to 5 fractions. Ten out of the 13 patients had SRS to the surgical cavity, while 2 received primary SRS and 1 patient had surgery to the largest metastasis followed by SRS to the surgical cavity and the other non-resected lesions. The average treated volume was 13.887cm3 (0.325 - 34.393), the maximum number of lesions treated was 3. Ten patients (35.7%) went on to have further SACT post SRS with 4 of the 10 patients receiving 2 lines of SACT. In SRS group (n=13), 7 relapsed within the brain, none of which relapsed within the radiotherapy fields. Of those relapsed patients, 2 received further SRS and 1 patient underwent surgery. Patients relapsed within 4 to 19 months, with 57.1% relapsing within 4 to 5 months and 42.9% relapsing after more than 9 months.
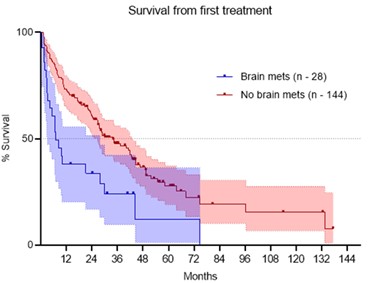
Median overall survival (OS) from first treatment (BDT or SACT) in patients with brain metastasis vs without was 6.9 vs 34 months respectively (P value = 0.0005, HR =2.23, 95% CI 1.20 -4.13).
Conclusion
BM is common in mRCC and symptomatic detection is often late leading to BSC only. We suggest regularly imaging surveillance for early detection and BDT. SRS is highly effective in local control of treated lesions however relapse outside SRS field is common. BM is a poor prognostic indicator despite BDT and SACT consistent with literature. Further study into pattern of failure and best sequence of SACT on survival is needed.