Mean age was 59 years and mean lesion was 18mm (9-25mm).
Primary tumor histology: NSCLC 51%, breast 25%, melanoma 8%, kidney 5%, colorectal 4%, other 7%.
RPA classification: I 48% and II 52%.
49% had received previous local treatment; 67% WBRT, 23% surgery and 10% WBRT+surgery.
62% received SF-SRS. Dose administered: 15Gy 88%, 18Gy 10% and 2% other dose.
38% received MF-SRS. Dose administered: 35Gy (7x5Gy) 62%, 30Gy (6x5Gy) 25% and 13% other dose.
There were no significant differences between SF-SRS and MF-SRS in terms of age, lesion , sex, histology or RPA.
Regarding previous local treatment, surgery was more frequent in MF-SRS (13% vs 3%) and WBRT in SF-SRS (27% vs 7%) (p=0.01).
RN was observed in 19% of patients, with a median time of appearance of 6 months (3.5-16) post-treatment.
85% of RN occurred in the SF-SRS group and 15% in the MF-SRS group (p=0.01).
The mean PTV volume of the lesions that developed RN was 4cc, with a compliance index of 1.7, isocenter dose mean 17.6Gy and marginal dose mean 14.6Gy.
44% of RN occurred in lesions between 10-20mm, 32% in those greater than 20mm and 24% in those less than 10mm.
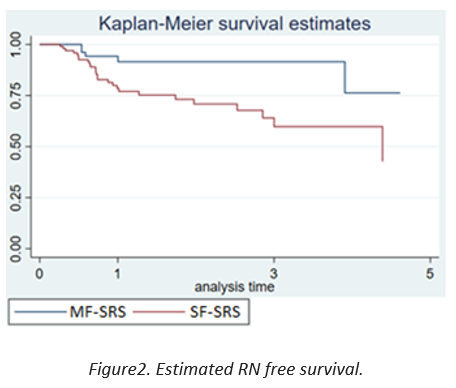
Using a ROC curve and the Youden`s index, the area under the lesion curve was 0.507 (0.402-0.612, p=0.05). The cut-off point was 15mm, with a sensitivity and specificity of developing RN of 68% and 46% respectively.
53% of RN were symptomatic; 83% of the RN in the MF-SRS group and 46% of the RN in the SF-SRS group.
Univariate analysis showed that receiving SF-SRS (OR 3.5, 1.4-9) or prior WBRT (OR 5.2, 1.1-24.1) were predictors of developing RN.
We found no relationship between histology or dose received and RN (p=0.8).
Patients with RN had higher V10 mean and V12 mean, but without significant differences: V10 10cc vs 8cc and V12 7cc vs 6cc.
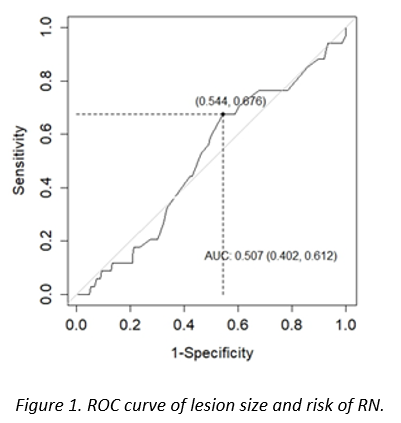
After a median follow-up of 4 years, the median OS was 2.5 years (1-5) and the median RN free survival was 2.8 years (1.8-5.4).
The estimated RN free survival in the MF-SRS group at 1, 3 and 5 years was 94% (8-98), 91% (78-96) and 76% (34-93) and in the SF-SRS group was 78% (68-85), 64% (49-76) and 42% (20-63) respectively (p=0.02).