Could Blood tests have prognostic value in Glioma patients? A mono-institutional experience
PO-1443
Abstract
Could Blood tests have prognostic value in Glioma patients? A mono-institutional experience
Authors: Marco Lucarelli1, Marianna Trignani1, Marzia Borgia1, Rosario Bonelli1, Antonietta Augurio1, Maria Taraborrelli1, Domenico Genovesi1
1"SS Annunziata" Hospital, "G. D'Annunzio" University, Radiation Oncology Unit, Chieti, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Glioma are malignant brain tumors and their higher-grade type, glioblastoma (GBM) is characterized by low survival time. In such a severe pathology, it can be important to select markers to predict outcomes. Chronic inflammation is a well-known adverse factor because of the increase of blood supply and the creation of microenvironment. Baseline blood analysis can provide information about inflammation cells. Recently, the combinations of these markers, such as the neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), the lymphocyte-to-monocyte ratio (LMR), systemic immune inflammation index (SII) and systemic inflammation response index (SIRI) were demonstrated as effective prognostic indicators. Our aims is to see if combined ratios of blood cells could have a predictive value of survival time in diagnosed glioma.
Material and Methods
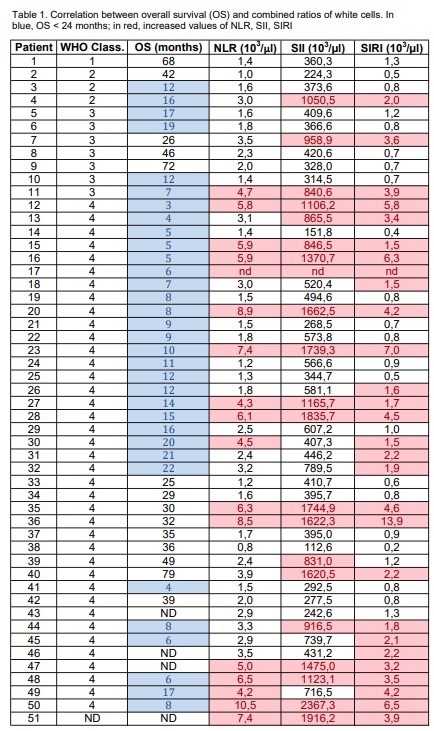
A retrospective analysis was carried out in patients with diagnosed glioma who underwent Radiotherapy between January 2016 and June 2022. The overall survival (OS) was defined as the interval between the diagnosis and death or, for patients still alive, between the diagnosis and their last follow-up. The pathological diagnoses were based on the classification of CNS tumors. Medical records were reviewed and patients and tumor data were collected. The expression of Ki-67 was categorized into two groups: low-intermediate (Ki-67 < 30%), and high (Ki-67 ≥ 30%). Blood tests results were collected before starting Radiation therapy. Hemoglobin, total white blood cells, neutrophils (N) platelets (P), lymphocytes (L) and monocytes (M) were collected. The NLR, the PLR, the LMR, the SII (P×N/L) and the SIRI (M×N/L) were calculated and compared to reference values.
Results
In our experience, 51 patients were analyzed. The median age was 58 ± 13 years old. The median of gliomas was 5 cm and 30% of them were multiple. Ki-67 ≥ 30% was registered in 30% for all WHO grades and in 80% for GBM. The median OS was 26 ± 18 months and patients with high-grade glioma were >80% of the analyzed group. All patients underwent Radiotherapy and >50% received a conventional schedule of 60 Gy (2Gy/fx). Temozolomide was given concomitantly to >80% of patients. Among blood variables, hemoglobin, lymphocytes, monocytes and platelets did not show significant changes. Neutrophils were increased in >30% of patients. In >30% of whole patients, NLR, SII and SIRI exceeded the reference values and in >40%, >50%, > 60% of GBM patients, NLR, SII and SIRI were significantly elevated, respectively. Moreover, increased NLR, SII, SIRI were in >30%, >40%, >50% of patients with ≤ 2 years OS respectively. PLR and LMR were within the reference ranges and did not differ significantly in GBM group.
Conclusion
Despite the small sample , as showed in a respective Polish study on 358 patients, our analysis seems to suggest that combined ratios of blood cells could have prognostic implications with the perspective of increasing personalized therapies for glioma patients.