Improving immunotherapy outcome in solid tumor by combining with other established cancer treatments
PO-2238
Abstract
Improving immunotherapy outcome in solid tumor by combining with other established cancer treatments
Authors: Priyanshu Sinha1, F. Charlemagne Asonganyi2, Søren Nygaard3, Mateusz K Sitarz4, Pernille B Elming1, Michael R Horsman1
1Institute of Clinical Medicine, Experimental Clinical Oncology - Dept. Oncology , Aarhus, Denmark; 2Institute of Clinical Medicine , Experimental Clinical Oncology - Dept. Oncology, Aarhus, Denmark; 3Institute of Clinical Medicine, Experimental Clinical Oncology - Dept. Oncology, Aarhus, Denmark; 4Institute of Clinical Medicine, Danish Centre of Particle Therapy, Aarhus , Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Introduction: There is great focus on establishing combinational therapies where radiotherapy or chemotherapy is given beforehand such that tumor becomes more immunogenic prior to administration of immunotherapy. This holds great importance for solid tumors, that are traditionally known to be poor candidates for immunotherapy. Our plan would be to investigate the combination of one such inhibitor (anti-CTLA-4; anti-cytotoxic T lymphocyte associated protein - 4) with treatments that have shown to have a bi-functional cell killing mechanisms. These include high dose proton radiation, and the vascular disrupting drug OXi4503, that not only have potential for tumor ablation, but also have shown to mediate tumor immunogenicity.
Objectives: To investigate the critical factors influencing the tumor growth inhibition seen when we combine anti-CTLA-4 with radiation, and vascular disrupting agent OXi4503.
Material and Methods
Materials & Methods: All experiments used C3H mammary carcinoma grown in the right rear foot of CDF1 mice. Treatments started when tumors were at specific s of 50, 100, 200, or 400 mm3. These included proton radiation (local tumor irradiation with 20 Gy on day 0), OXi4503 (50 mg/kg, injected i.p. on days 0, 3, 7, and 10), achieved by immersing the tumor bearing leg in a water-bath), and anti-CTLA-4 (injected i.p. on days 1, 4, 8, and 11). The endpoint was tumor growth delay (time to grow to 1000 mm3).
Results
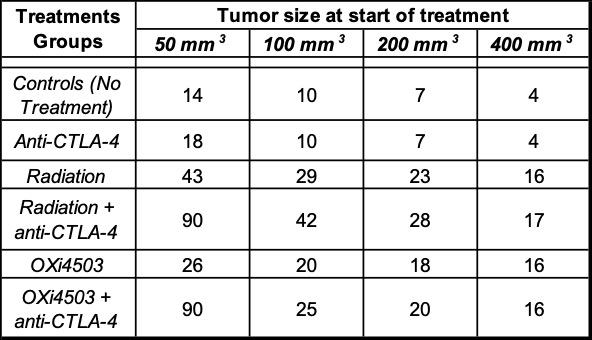
Results: Median time (days) taken for tumors to reach 1000 mm3 for different treatment groups are shown in the Table 1 below.
Conclusion
Conclusions: Our Tumor model is generally unresponsive to Anti-CTLA-4 as a single therapy agent, even though an effect could be observed in the smallest size tumors. An enhanced response was obtained when it was combined with either proton radiation or OXi4503. With increasing the of primary tumor size at treatment, the benefit of combinational therapy decreases, indicating negative co-relation between tumor size at treatment and the resulting efficacy of the combination therapy. There is a possibility of the enhancement being strongly dependent on the extent of damage done prior to anti-CTLA-4 treatment and further investigations are bing carried out to determine the minimum damage for the combination therapy to be effective in smaller size primary tumors.
This project has received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement No 955625 (Hyperboost; www.Hyperboost-h2020.eu) and a grant from the Danish Cancer Society.