Low dose fractionated radiotherapy enhances immunotherapy treatment outcomes
PO-2236
Abstract
Low dose fractionated radiotherapy enhances immunotherapy treatment outcomes
Authors: Rebecca D'Alonzo1,2,3, Synat Keam2,3,4, Kelly MacKinnon1,2,3, Alistair Cook2,3,5, Anna Nowak2,3,4, Suki Gill6, Pejman Rowshanfarzad1, Martin Ebert1,6,7
1University of Western Australia, School of Physics, Mathematics and Computing, Perth, Australia; 2University of Western Australia, National Centre for Asbestos Related Diseases, Perth, Australia; 3University of Western Australia, Institute for Respiratory Health, Perth, Australia; 4University of Western Australia, Medical School, Perth, Australia; 5University of Western Australia, School of Biomedical Sciences, Perth, Australia; 6Sir Charles Gairdner Hospital, Australia, Department of Radiation Oncology, Perth, Australia; 75D Clinics, 5D Clinics, Perth, Australia
Show Affiliations
Hide Affiliations
Purpose or Objective
Malignant tumours have decreased oxygenation due to malformed blood vessels. The hypoxia decreases the effectiveness of radiotherapy (RT), and the abnormal blood vessels prevent both systemic therapies and immune cells from reaching areas of the tumour. This study built upon our previous research, where it was found that 2 Gy x 5 fractions achieved and maintained tumour vasculature normalisation and reoxygenation for a week post-irradiation. This RT fractionation treatment plan was combined with various immunotherapy schedules to identify the RT plus immunotherapy combination that has the greatest synergistic effect and improves treatment outcomes.
Material and Methods
BALB/c mice were subcutaneously injected with AB1-HA mesothelioma tumour cells. Mice with established tumours received 2 Gy per day for 5 consecutive days, starting 10 days post-inoculation. Mice also received various schedules of immune checkpoint inhibitors (anti-PD-1 and anti-CTLA-4). Tumours were monitored and mice that had a complete response, determined by no observable primary tumour for 30 days, then underwent tumour rechallenge with the same cell line.
Results
The combination of RT + anti-PD-1 significantly improved survival compared to anti-PD-1 alone. When anti-PD-1 was given concurrently with RT, half the mice had a complete response. The addition of anti-CTLA-4 to the treatment schedule significantly increased survival compared to both RT + anti-PD-1 and anti-PD-1 + anti-CTLA-4. All mice that received concurrent delivery of RT + anti-PD-1 + anti-CTLA-4 had a complete response. Cured mice resisted tumour rechallenge, regardless of the original treatment group.

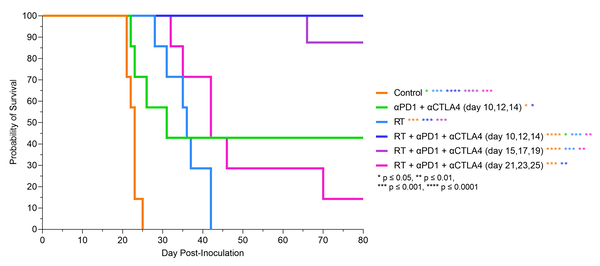
Conclusion
The effects of 2 Gy x 5 fractions on the tumour microenvironment significantly improved the treatment outcomes of immune checkpoint inhibitors in murine models of mesothelioma. Concurrent delivery of RT + anti-PD-1 + anti-CTLA-4 resulted in 100% of primary tumours being cured. Gained immunity to the cell line was produced by all mice that had a complete response.
Acknowledgements
This study was supported by grant 1163065 from the Cancer Australia Priority-driven Collaborative Cancer Research Scheme. I would like to thank the Sir Charles Gairdner Hospital Radiation Oncology Scholarship in Radiobiology for their support.