Optimisation and dose calculation differences between algorithms in endometrial brachyterapy
Sergio Honorato Hernandez,
Spain
PO-2180
Abstract
Optimisation and dose calculation differences between algorithms in endometrial brachyterapy
Authors: Sergio Honorato Hernandez1, David Hernandez Gonzalez1, Pablo Castro Tejero1, Pablo Chamorro Serrano1, Maria Roch Gonzalez1, Rocio Simon de Blas1, Maria Sol Talaya Alarcon2, Sara Carroceda Gonzalez2, Aranzazu Valiente Gonzalez2
1H. U. La Princesa, Medical Physics, Madrid, Spain; 2H. U. La Princesa, Radiation Oncology, Madrid, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
The publication 10 years ago of TG186 has been thanks to the development of the model-based dose calculation algorithms (MBDCA) for brachytherapy, which have been further developed in recent years.
Heterogeneity correction algorithms are used in external radiotherapy several years ago, however in brachytherapy are now beginning to use in Clinical practice.
This work shows the differences, both inverse optimisation and dosimetric, between the calculation with TG43 and AcurosXB (AX) in brachytherapy treatment for endometrial cancer.
Material and Methods
For the analysis of the inverse optimisation, the VEGO TG-43 (TG-43 Opt.) and Acuros BV (AX Opt.) volume optimisations were used, analysing the source time at each stop position, using 100% coverage at 100% dose and 5% coverage at 105% dose to the reference line, located 5 mm from the surface of the applicator, with priority 100 and smoothing of 153.
For the dosimetric analysis, CTV coverage and dose to OARs were analysed in 46 patients treated in a Varian BRAVOS brachytherapy unit, using the TG-43 and AX dose calculation (DC) algorithms. The diameter of the applicators used was 2.5, 3 and 3.5 cm and the fractionation of treatments was two fractions of 5.5 Gy and three fracions of 5Gy in non-exclusive brachytherapy and three fractions of 7 Gy in exclusive brachytherapy.
For both the inverse optimisation and the dosimetric study, the Varian Brachyvision planning system was used.
Results
The total treatment time is, on average, 1.54% longer when using AX Opt., with differences of up to 4.81%.
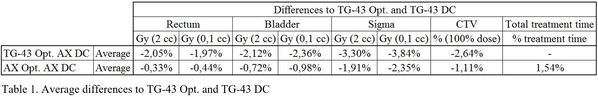
AX Opt. and AX DC implies an average underdose versus TG-43 Opt. and TG-43 DC of 1.11% for CTV coverage with 100% dose, 0.33%, 0.72% and 1.91% for D(2 cc) and 0.44%, 0.98% and 2.35% for D(0.1 cc) in rectum, bladder and sigma, respectively, finding maximum differences of up to 3.7% in CTV coverage, 3.42%, 3.37% and 4.55% for D(2 cc) and 3.61%, 4.35% and 5.23% for D(0.1 cc) in rectum, bladder and sigma, respectively.
Regarding the differences found solely due to the calculation algorithm (using TG-43 Opt. in both cases) with AX DC we found an average underdose versus TG-43 DC of 2.64% for 100% coverage of CTV with 100% of the prescription dose, 2.05%, 2.12% and 3.30% for D(2 cc) and 1.97%, 2.36% and 3.84% for D(0.1 cc) in rectum, bladder and sigma, respectively, finding maximum differences of up to 6.2% in CTV coverage, 3.53%, 3.42% and 4.9% in D(2 cc) and 4%, 4.16% and 5.48% in D(0.1 cc) in rectum, bladder and sigma respectively.
The results are shown in Table 1.
Conclusion
Both the TG-43 Opt. and the TG-43 DC algorithm overestimate the dose reaching the CTV and OARs because it does not take into account the heterogeneities in the patient and the dose attenuation occurring in the applicator itself.
The AX Opt. as well as the AX DC algorithm are closer to reality, obtaining discrepancies compared to the traditional calculation.