Temperature effect on optical fibre sensors for in-vivo dosimetry in HDR brachytherapy
Owen Mc Laughlin,
United Kingdom
PO-2179
Abstract
Temperature effect on optical fibre sensors for in-vivo dosimetry in HDR brachytherapy
Authors: Owen Mc Laughlin1, Sergio Esteve2, Orla Houlihan1,3, Geraldine Workman2, Monica Byrne2, Suneil Jain1,3, Alan Hounsell2,1, Kevin Prise1, Conor McGarry1,2
1Queen's University Belfast, Patrick G Johnston Centre for Cancer Research, Belfast, United Kingdom; 2Belfast Health and Social Care Trust, Radiotherapy Physics, Northern Ireland Cancer Centre, Belfast, United Kingdom; 3Belfast Health and Social Care Trust, Department of Clinical Oncology, Northern Ireland Cancer Centre, Belfast, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Optical fibre sensors are a component of an in-vivo dosimetry system developed by the EU funded H2020 program “Origin” for source localization and dose measurement during prostate and gynaecological HDR brachytherapy procedures. It is essential to establish the effect of temperature change on dose measurements due to the possible temperature differences between calibration set up and clinical use.
Material and Methods
Sensors consist of a 1Y2O3:Eu+4YVO4:Eu and PMMA tip coupled to a polymer optical fibre. Output measurements are obtained with a 16 silicon photomultiplier (SiPM) array. Measurements with a 5 cm source-sensor distance were taken using a custom Perspex water tank adapted to hold the optical fibre dosimeters and the afterloaded Ir-192 Flexisource within 6F Elekta Proguide needles. An equivalent exposure time of 10 seconds for a 40,000 cGy cm2/h source strength was used. Detector output in photon counts per second was averaged for the exposure time with the dark count rate subtracted. Statistical uncertainty and reproducibility were quantified using three repeated measurements at one temperature.
Detector temperature dependence was evaluated by placing 14 optical fibres in a water filled plastic vessel with a magnetic stirrer at an initial temperature of 39.6°C. The Perspex water tank was filled with cold water and an icepack to induce cooling to room temperature at 26.7°C. Dosimeter temperature was monitored outside the treatment room using a DS18B20 temperature sensor connected to an Arduino Nano, with the source being deployed when a temperature change of 1°C was recorded.
Results
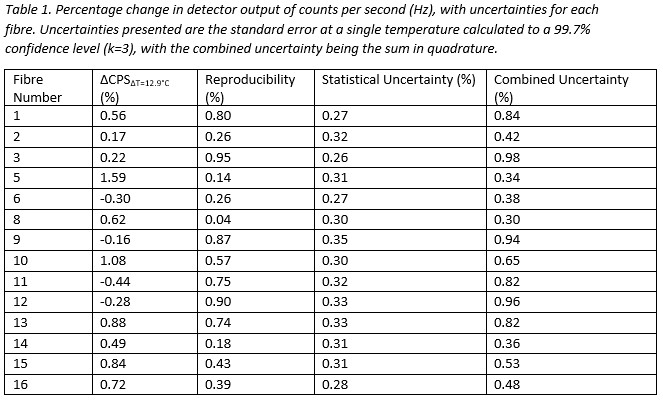
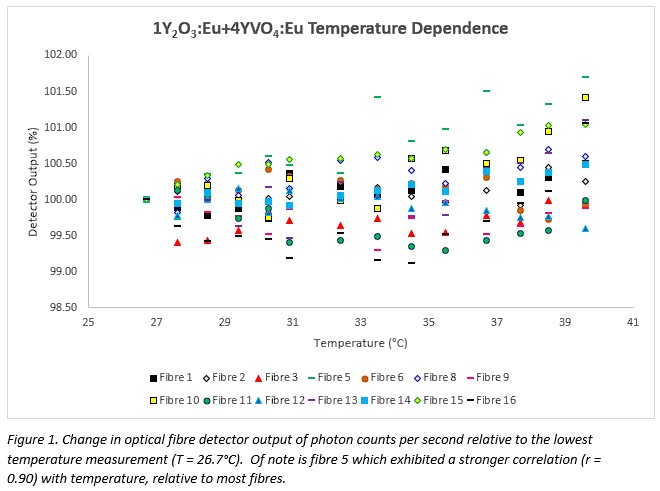
Applying a linear regression model and averaging the change in count magnitude between temperatures of 26.7°C and 39.6°C for fourteen fibres results in a total change in detector output of 0.43% with a standard error of 0.47% (k = 3). The combined uncertainty of the statistical noise in photon counting and the reproducibility for each detector is presented in table 1. Two fibres are excluded due to a sensor and SiPM fault. For a total of 196 measurements for all fibres, 47 exceeded the measurement uncertainty.
Conclusion
The change in dosimeter output with temperature in the range of 26.7°C to 39.6°C was found to vary between fibres. The low average change in output suggests the scintillator is useful for in-vivo applications. A method of evaluating temperature dependence is outlined which minimises the influence of positional uncertainty on measurements, which is essential when using small volume detectors with a brachytherapy source.
Funding statement
The ORIGIN project is an initiative of the Photonics Public Private Partnership (www.photonics21.org), and has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 871324. Authors are also supported by the Research and Development Division of the Public Health Agency of NI (COM/5610/20).