Implementation and validation of TG-43 table-based dose calculations in RapidBrachyMCTPS
Jonathan Kalinowski,
Canada
PO-2173
Abstract
Implementation and validation of TG-43 table-based dose calculations in RapidBrachyMCTPS
Authors: Jonathan Kalinowski1,2, Shirin Enger3,2
1McGill University , Medical Physics Unit, Department of Oncology, Montreal, Canada; 2Jewish General Hospital, Lady Davis Institute for Medical Research, Montreal, Canada; 3McGill University, Medical Physics Unit, Department of Oncology, Montreal, Canada
Show Affiliations
Hide Affiliations
Purpose or Objective
RapidBrachyMCTPS is a brachytherapy treatment planning system (TPS) built upon a Monte Carlo (MC) dose calculation engine. Dose to patient medium is determined beyond the TG-43 formalism by simulating radiation transport inside a reconstruction of the patient with accurate assignment of tissue material and density. However, knowledge of dose to water (Dw) remains desirable for its simplicity, reproducibility, and comparability with clinical dosimetry. Currently, calculation of Dw for patients has only been performed with the MC method in RapidBrachyMCTPS. This work aims to optimize Dw calculation in RapidBrachyMCTPS by implementing a lookup-table based TG-43 dose calculation as performed in clinical brachytherapy TPS to enable comparison with clinically planned dose.
Material and Methods
Benchmarking of TG-43 Dw calculation in RapidBrachyMCTPS was performed by comparison with MC Dw for an Ir-192 breast brachytherapy case with 144 dwell positions. A dose grid with 1 mm³ voxels was selected for both methods. MC simulations were run on a CPU cluster with 40 cores, while TG-43 calculations were performed locally on a personal computer with 16 CPU cores.
Results
A comparison of the TG-43 versus MC Dw is shown in Table 1. DVH metrics for the PTV and OARs for this plan agreed within 1%, except the skin D2cc when TG-43 dose was calculated only inside the body contour. This discrepancy is due to the presence of voxels in the skin contour that lie outside of the body contour. A gamma index comparison between TG-43 full and MC dose distributions yielded a pass rate of 99.3% with a 1%/1 mm criterion, indicating good agreement. The lookup table-based TG-43 calculation accelerated the dose by a factor of about 66 and 290, when dose outside the body contour was included or excluded, respectively.
Table 1:
| Metric | TG43 Dw Full / TG43 Dw Body Only | MC Dw | %difference |
| PTV D90 [Gy] | 3.619 | 3.644 | 0.7 |
| Heart D2cc [Gy] | 1.456 | 1.454 | 0.1 |
| Chest Wall D2cc [Gy] | 2.658 | 2.675 | 0.6 |
| Skin D2cc [Gy] | 2.754 / 2.729 | 2.772 | 0.6 / 1.5 |
| Calculation Time [s] | 127 / 29 | 8416 | - |
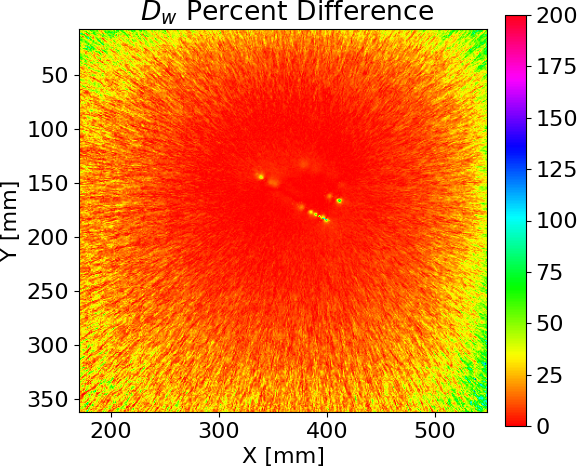
Figure 1 displays the percent difference between the TG-43 full and MC Dw distributions on the central transverse slice of the patient. Discrepancies can be seen at the periphery due to the large statistical uncertainty in MC dose far from the source. Voxels near the source also display significant deviation due to the breakdown of the TG-43 formalism at distances less than the source’s active length. TG-43 and MC Dw show agreement between these extremes, though MC Dw may be necessary when accurate determination of dose near sources is needed.
Figure 1:
Conclusion
TG-43 Dw may now be calculated faster and accurately in RapidBrachyMCTPS in lieu of MC simulations. Further benchmarking of TG-43 dose calculations in RapidBrachyMCTPS will be completed with different sites and will be validated against dose calculations from clinical TPS.