Optimization of catheter placement for transperineal interstitial gynaecological brachytherapy
PO-2156
Abstract
Optimization of catheter placement for transperineal interstitial gynaecological brachytherapy
Authors: Jillian Bennett1, Cédric Bélanger2,3, Philippe Chatigny2, Luc Beaulieu2,3, Alexandra Rink4,1,5
1University of Toronto, Department of Medical Biophysics, Toronto, Canada; 2l’Université Laval, Département de physique, de génie physique et d’optique et Centre de recherche sur le cancer, Québec City, Canada; 3CHU de Québec - Université Laval, Département de radio-oncologie et Centre de recherche du CHU de Québec, Québec City, Canada; 4University Health Network, TECHNA Institute, Toronto, Canada; 5University of Toronto, Department of Radiation Oncology, Toronto, Canada
Show Affiliations
Hide Affiliations
Purpose or Objective
Brachytherapy (BT) is an essential pillar in the treatment of cervical cancer. However, there are currently no established guidelines regarding the optimal number and placement of interstitial (IS) gynaecological (GYN) BT catheters. One method of IS GYN BT uses a transperineal catheter-guiding template in combination with an intrauterine (IU) tandem. Typically, catheter locations are decided based on pre-BT imaging, and radiation treatment plans are then determined based on imaging taken after catheter insertion. This can lead to suboptimal tumor coverage, and often unused catheters, which contribute to increased implantation time and tissue injury. Instead, changes to patient anatomy due to the IU tandem suggest that images taken after insertion of the Tandem and APPlicator (post-TAPP) may be better suited than pre-BT images for catheter planning.
In previous studies on prostate BT, the use of catheter optimization algorithms could quickly produce equivalent or superior treatment plans using fewer IS catheters compared to clinical cases. To verify these findings for GYN BT, we implemented a Centroidal Voronoi Tessellation (CVT) algorithm for catheter optimization in prior cervix cancer cases. CVT uniformly distributes a given number of catheters throughout a 2D projection of the target volume. We therefore hypothesize that using CVT for catheter planning on post-TAPP MRI will improve or maintain treatment plan quality with fewer catheters.
Material and Methods
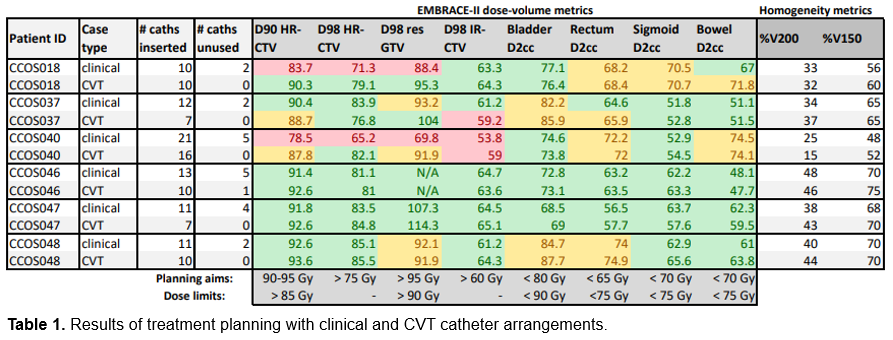
Cases of locally advanced cervical cancer treated from 2017 to 2019 using IS BT with a Syed Neblett template were selected (N=6). Target, organ-at-risk (OAR), and clinical catheter delineations were retrieved from post-insertion imaging. CVT was used to simulate post-TAPP optimized catheters for each case. Treatment plans were then generated by a single expert for both the CVT and clinical catheter arrangements. Plan quality was evaluated via compliance with the clinically used EMBRACE-II dose-volume constraints. Measures of dose inhomogeneity (%V150 and %V200) were also recorded.
Results
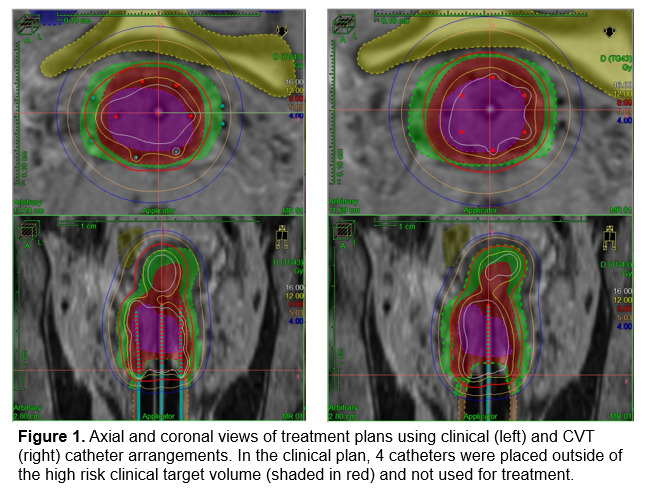
In all cases but 1, the CVT arrangements produced improved or EMBRACE-II compliant treatment plans with as many or fewer inserted catheters compared to the clinical cases (Table 1). A small increase in %V150 was observed between sample groups (p < 0.05). Additionally, the clinical cases resulted in 20 total unused catheters (ex. Fig. 1), while those with CVT had only 1 total. 2 plans using clinical catheters failed to meet target dose minimums, and thus would have required a new implant in clinical practice; however, the plans using CVT catheters for the same patients met all, and all but 1, clinical objectives respectively.
Conclusion
This preliminary retrospective work supports the hypothesis that CVT with post-TAPP imaging can achieve clinically acceptable dose distributions while limiting insertion of extraneous catheters. Future work aims to increase the cohort size and further quantify the effect of lowering the number of CVT catheters.