Dosimetric uncertainties due to inter-fraction organ at risk movement in HDR cervical brachytherapy.
Orla Houlihan,
United Kingdom
PO-2142
Abstract
Dosimetric uncertainties due to inter-fraction organ at risk movement in HDR cervical brachytherapy.
Authors: Orla Houlihan1,2, Monica Byrne3, Owen McLaughlin3,2, Geraldine Workman3, Sergio Esteve3, Conor McGarry3, Ursula McGivern1, Anne Drake1, Elizabeth Baird1, Kevin Prise2, Alan Hounsell3, Suneil Jain1,1
1Northern Ireland Cancer Centre, Belfast Health and Social Care Trust, Clinical Oncology, Belfast, United Kingdom; 2Queen's University Belfast, Patrick G. Johnston Centre for Cancer Research, Belfast, United Kingdom; 3Northern Ireland Cancer Centre, Belfast Health and Social Care Trust, Radiotherapy Medical Physics, Belfast, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
To investigate the requirement for in vivo dosimetry in HDR cervical brachytherapy by assessing the effect of inter-fraction organ at risk (OAR) movement on dosimetric parameters and to identify the OAR subsections which experienced the most dosimetric variation with the view to determining the optimal positions for in vivo dosimeters during brachytherapy.
Material and Methods
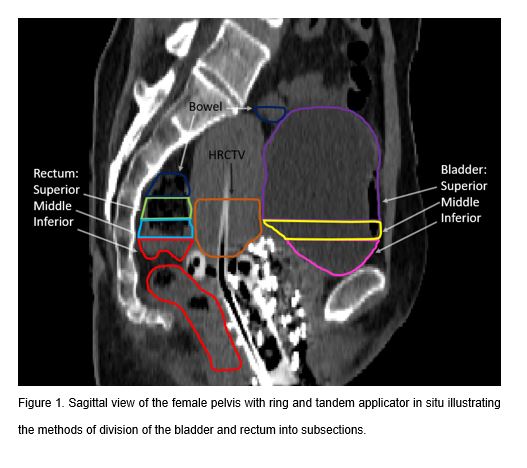
20 consecutive patients who underwent three fractions of MRI/CT-guided brachytherapy prescribed to Point A (2 cm above and lateral to the cervical os, perpendicular to the uterine axis) as part of radical treatment for cervical cancer were included. Organs at risk (OARs) of interest were bladder, rectum and bowel. The bladder and rectum were divided into subsections of superior, middle and inferior along divisions of the upper, middle and lower third of the high risk clinical target volume (HRCTV) (Fig. 1). Dosimetric parameters for each OAR and subsection were calculated for the pre-fraction 2 and 3 CTs and compared to the pre-fraction 1 CT.
Results
The mean differences (± standard deviations) of the D2cc (minimum dose to the most irradiated 2cc) of the pre-fraction 2 and 3 CTs compared to the pre-fraction 1 CT were -23.5% (±38.7%), -8.4% (±32.4%) and -2.2% (±19.3%) for the superior, middle and inferior bladder respectively and 7.3% (±49.2%), 7.3 (±30.3%) and 7.5% (±28.5%) for the superior, middle and inferior rectum respectively. Percentage deviations in D2cc for bladder subsections ranged from -100% to 28.1% (superior), -100% to 89.1% (middle) and -44.5% to 97.2% (inferior). Percentage deviations in D2cc for rectum subsections ranged from -100% to 126.8% (superior), -48.4% to 111.9% (middle) and -25.9% to 107.4% (inferior).
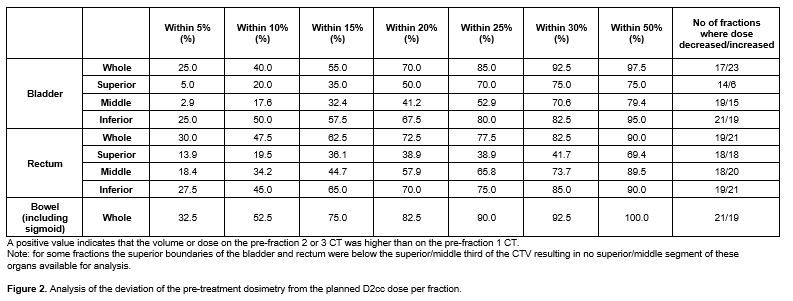
The D2cc of the pre-fraction 2 and 3 CTs were within 10% of the pre-fraction 1 CT D2cc dose in 20%, 17.6% and 50% of fractions for superior, middle and inferior bladder respectively and within 10% in 19.5%, 34.2% and 45% of fractions for superior, middle and inferior rectum respectively (Fig. 2). At a prescription dose of 7Gy for each fraction, the bladder dose constraint of 90GyEQD2 (α/β=3) was exceeded in 40% (8/20) of treatment courses and the rectum and bowel dose constraint of 75GyEQD2 (α/β=3) was exceeded in 45% (9/20) and 50% (10/20) treatment courses respectively. To keep the dose to OARs within acceptable constraints, dose reduction was required for all three brachytherapy fractions in 35% (7/20) of patients, for two fractions in 15% (3/20) of patients and for one fraction in 15% (3/20) of patients with no dose reduction required for 35% (7/20) of patients.
Conclusion
Inter-fraction OAR motion occurs in cervical brachytherapy and can necessitate prescription dose reduction. The superior and middle subsections of the rectum and bladder experienced the greatest percentage deviations on the pre-fraction 2 and 3 CTs compared to the pre-fraction 1 CT. Dosimeters should be placed in a range of locations within the rectum and bladder at the level of the HRCTV.