Analysis of the Interplay Effect in Lung SABR Based on Breathing Motion and Plan Characteristics.
ASMAA ALI,
United Kingdom
PO-1881
Abstract
Analysis of the Interplay Effect in Lung SABR Based on Breathing Motion and Plan Characteristics.
Authors: ASMAA ALI1,2, Jason Greenwood1, Mohammad Varasteh3, Sergio Esteve2, Prakash Jeevanandam2, Fabian Göpfert4, Denise Irvine2, AR. Hounsell2,3, CK. McGarry2,3
1Queen’s University Belfast, School of Mathematics and Physics, Belfast, United Kingdom; 2Belfast Health and Social Care Trust, Radiotherapy Physics, Belfast, United Kingdom; 3Queen’s University Belfast, Patrick G Johnston Centre for Cancer Research, Belfast, United Kingdom; 4PTW, PTW, Freiburg, Germany
Show Affiliations
Hide Affiliations
Purpose or Objective
The delivery of stereotactic ablative radiotherapy doses is susceptible to challenges for tumour motion in the thoracic region. This study aims to investigate the effect of breathing characteristics and plan complexity in the interplay effect.
Material and Methods
Thirteen lung SABR plans were nominated for patient-specific interplay effect evaluation via in-house software in conjunction with an alpha version of the treatment plan verification software verisoft (PTW-Freiburg, Germany). The dose distribution of a virtual moving phantom was simulated using the static phantom dose measurements acquired using the OCTAVIUS 4D phantom (PTW-Freiburg, Germany). The influence of plan complexity, number of breaths per delivery (NBs), motion amplitudes, and Planning Target Volume (PTV) in the interplay effect were examined. The modulation complexity score (MCS) was used as the plan complexity metric. User-defined NBs per irradiation ranging from (5 to 50) were calculated for each plan. The influence of breathing amplitude was examined using a sinusoidal pattern in the superior-inferior direction with an extent ranging from (0 mm to 25 mm). The dose distribution of two breathing extremes 0% and 50% were considered to demonstrate the extreme interplay scenarios. A total of 2100 plans were analysed using the gamma criteria of 2%/2mm with 10% and 50% thresholds. A multiple regression model was used to assess the relationship of the NBs, amplitude, PTV , and MCS with gamma pass rates.
Results
Figure 1 shows that there was a strong correlation between the motion amplitude (p<0.01) and the NBs (p<0.01). Increased NBs reduce the interplay effect for high motion amplitudes. There was an absence of correlation between the gamma passing rate and the PTV (p=0.25) and MCS (p=0.10). Gamma pass rates <90% became evident at 5-20 NBs with amplitudes > 5mm Figure 1 B.
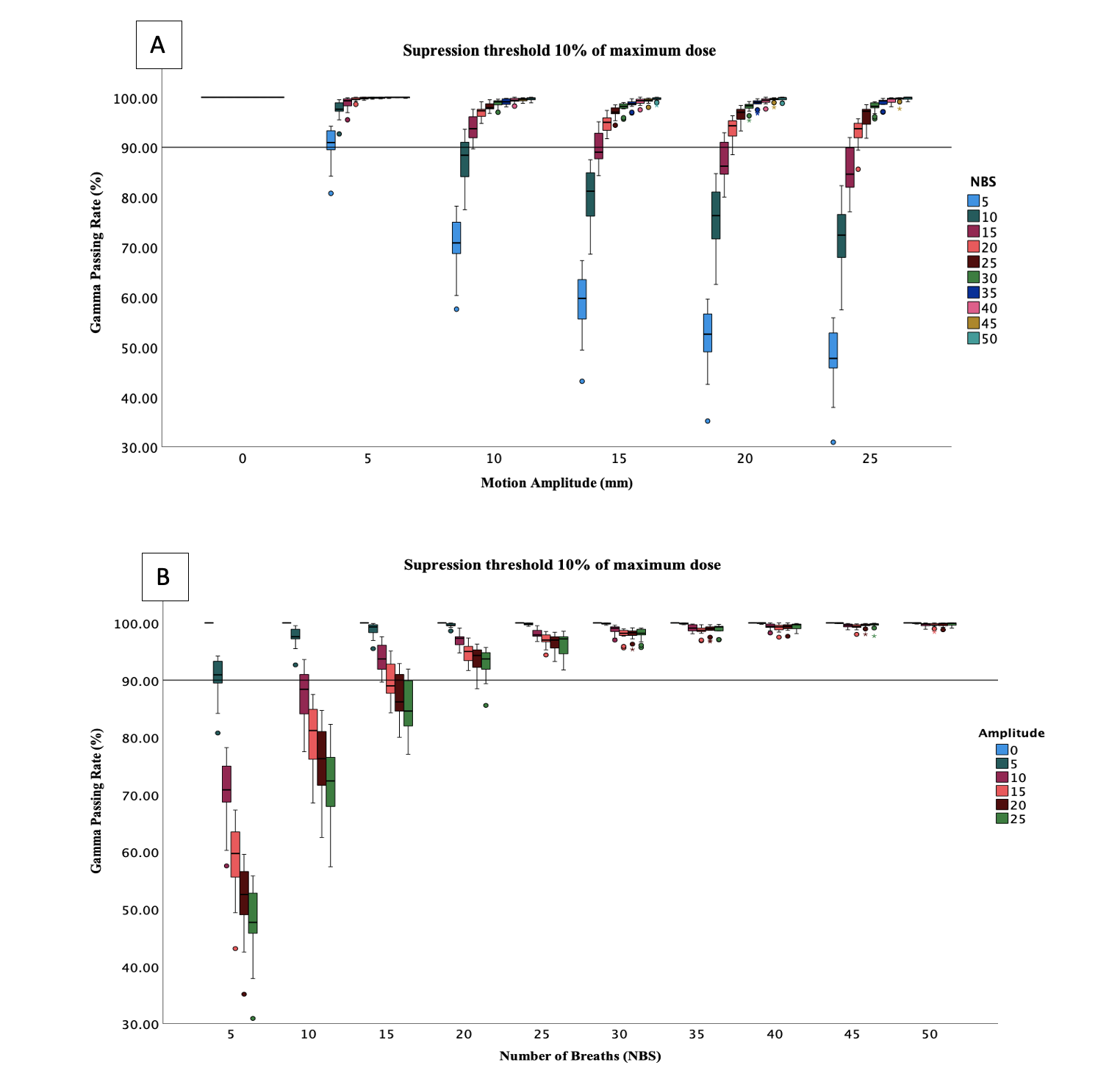
Figure 1: A box plot of the gamma passing rate (phase 0% vs phase 50%) of all 13 plans using the gamma analysis criteria (2%/2mm) as a function of the NBs (A) and motion amplitude (B) with 10% thresholds. The solid line represents the 90% gamma passing rate.
Conclusion
High interplay effects were observed for long breathing periods (less NBs) with extended motion amplitudes. It is recommended that treatment plans for patients with these features should include motion management techniques such as gating or breath-holding to improve treatment precision and, consequently, treatment outcomes.