Full course 4D IMPT dose assessments for thoracic targets with large motion
Sabine Visser,
The Netherlands
PO-1863
Abstract
Full course 4D IMPT dose assessments for thoracic targets with large motion
Authors: Sabine Visser1, Erik W. Korevaar1, Robin Wijsman1, Christina T. Muijs1, Johannes A. Langendijk1, Pietro Pisciotta1, Gabriel Gutteres Marmitt1, Cássia O.Ribeiro1, Stefan Both1
1UMCG, Radiotherapy, Groningen, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Despite the dosimetric benefits of intensity-modulated proton therapy (IMPT), plan robustness may be compromised due to its sensitivity to treatment uncertainties. For target volumes located in the thorax, there is an additional uncertainty due to motion and interplay effects. Before clinical implementation, we investigated the robustness of our clinical protocol by simulating the treatment with the 4D robustness evaluation method (4DREM). In clinical context, we use a combination of 3D robustness evaluation (3DREM) and 4D dose reconstruction (4DREAL) throughout the patient’s treatment. In this study, we investigate plan robustness outcomes obtained with these three methods for thoracic targets with large motion treated at our proton centre.
Material and Methods
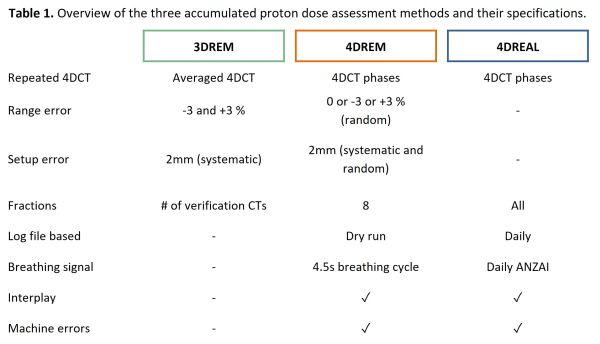
Layered rescanned (5x) 3D-robust optimised IMPT plans were generated on the averaged planning 4DCT for nine lung, one thymoma and ten oesophageal cancer patients with large target motion (>10mm). Plan adaptation was performed if target coverage degraded based on weekly 4DCTs. Full patient treatments including replanning were evaluated through 3DREM, 4DREM and 4DREAL, which all rely on dose deformation and accumulation based on multiple 4DCTs (Table 1). The 3DREM is based on averaged 4DCTs. 4DREM and 4DREAL split the treatment dose over the phases of the 4DCTs based on the time structure of beam delivery and a breathing pattern, to account for motion and interplay. The 4DREAL does this with daily inputs from the actual treatment, whereas 4DREM uses a standard breathing cycle and log files from a dry run, which can therefore be performed without fraction-wise data. Setup and range errors were only accounted for in 3DREM and 4DREM, which resulted in multiple treatment scenarios. Target coverage, mean lung dose (MLD) and mean heart dose (MHD) were investigated using the three methods.
Results
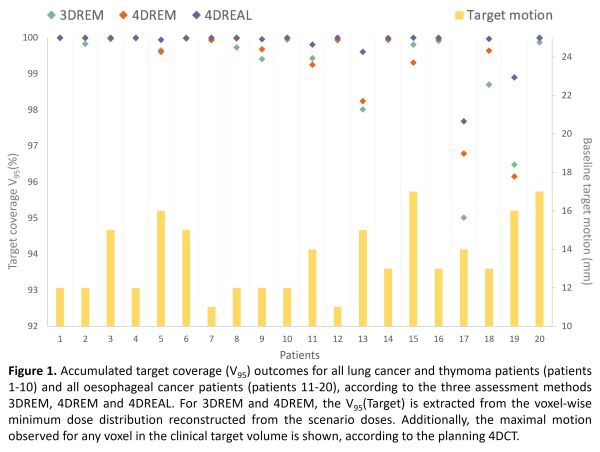
Baseline target motion for all patients ranged from 11–17mm (Figure 1). Plan adaptations were performed once for the lung cancer patients, and six times for the oesophageal cancer patients, mostly due to target deformations and diaphragm displacements. The target volume receiving 95% of the prescription dose (V95) was at least 95.0% in 3DREM, 96.2% in 4DREM and 97.7% in 4DREAL. The V95 was consistent between methods with 16/20 patients showing differences below 1%. 4DREAL showed the highest target coverage (99.8±0.6%, p<0.001), while no trends were observed between 3DREM and 4DREM (99.3±1.3% and 99.4±1.1%, p=0.268). No significant differences were observed between methods for MHD and MLD.
Conclusion
Rescanned IMPT was found to be suitable to treat thoracic tumours in free breathing for motion up to 17mm. Anatomical changes, range and setup errors had a more severe impact on target coverage than motion and interplay effects in a fractionated proton treatment. This confirms that the 3DREM can be safely used to quickly assess the need for replanning. Furthermore, the choice of evaluation method had no impact on organ-at-risk dose evaluation.