Image-guided IORT after surgical resection of brain malignancies: a feasibility study
Gustavo R. Sarria,
Germany
PO-1853
Abstract
Image-guided IORT after surgical resection of brain malignancies: a feasibility study
Authors: Gustavo R. Sarria1, Molina Grimmer1, Motaz Hamed2, Mohammed Banat2, David Koch1, Hektor Lorenzana2, Martin Fiebich3, Jasmin A. Holz1, Carsten Schmeel4, Ana Kowark5, Leonard C. Schmeel1, Stephan Garbe1
1University Hospital Bonn, Radiation Oncology, Bonn, Germany; 2University Hospital Bonn, Neurosurgery, Bonn, Germany; 3Technische Hochschule Mittelhessen, Bachelorstudiengang Medizinische Physik und Strahlenschutz, Giessen, Germany; 4University Hospital Bonn, Neuroradiology, Bonn, Germany; 5University Hospital Bonn, Neurosurgical Anesthesiology, Bonn, Germany
Show Affiliations
Hide Affiliations
Purpose or Objective
Intraoperative radiation therapy (IORT) can be used to locally apply radiation doses to surgical cavities of resected brain metastases and glioblastoma. The miniaturized linear accelerator INTRABEAM 600® (Carl Zeiss Meditec AG, Oberkochen, Germany) offers a low-energy system of 50kV X-rays. To date, placing the spherical applicator in the surgical bed has been done manually and without final positioning verification. Ultimately, without positional control, it must be assumed that the applicator is optimally positioned against the tissue in the tumor cavity, without any air interference or fluid underlying. Misplacements could lead to incomplete dose delivery, potentially yielding an increased risk of recurrence. Therefore, we deemed relevant to assess intraoperative imaging as a novel option for easing the applicator positioning.
Material and Methods
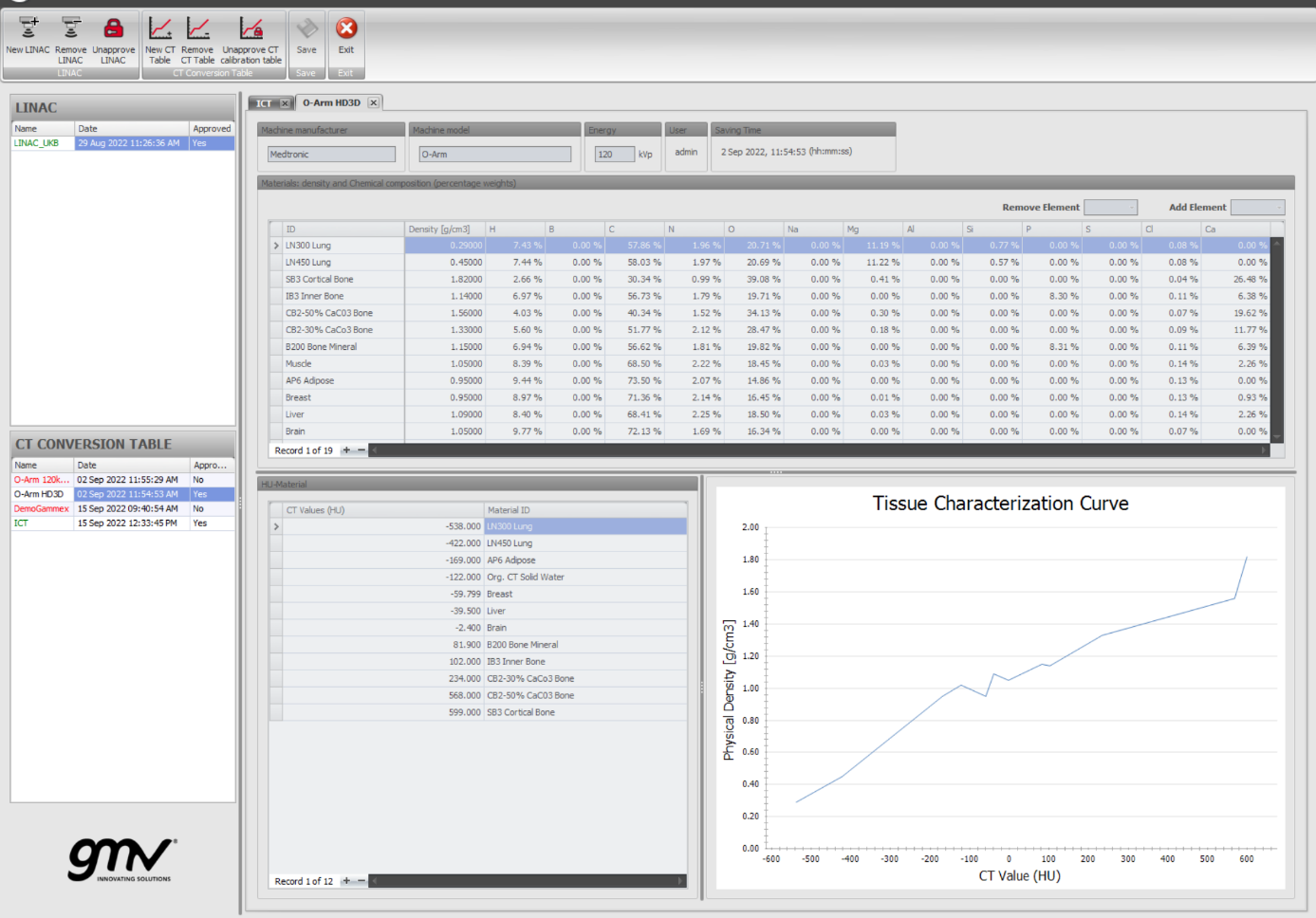
A surgical environment was mimicked in two test runs with an interdisciplinary team, accounting for operating and anesthesia times. The IORT planning software Radiance (GMV Innovating Solutions, Madrid, Spain) was previously calibrated with a “cheese” phantom, using twelve different density levels from 0.3 to 1.842 g/cm3, yielding a value-to-density table with -600 to +600 HU range. Furthermore, two inserts were placed in the phantom to evaluate the quality and spatial resolution of the cone-beam CT (CBCT) imaging. The O-Arm System (Medtronic, Minneapolis, MN, USA) was employed for acquiring tomographic intraoperative imaging, once the applicator was placed in a skull-shaped phantom. Two expert radiation oncologist contoured the acquired dataset and performed the treatment calculations, based on a 30 Gy prescription dose.
Fig 1. Head phantom, stereotactic device and O-arm system, mimicking a real surgical scenario.

Fig 2. Density tables acquired with the O-arm system, importen to Radiance for Monte Carlo planning
Results
We achieved the best possible CBCT imaging quality with the 120kV and 20mA setting parameters. This corresponds to the "HD3D (large)" O-Arm setting mode. With this, the image quality with artifact reduction, minimization of image noise and consideration of a low radiation exposure of only 0.5mSv for the patients is feasible. Approximately 15 additional minutes were accounted for contouring and planning times.
Conclusion
Good-quality intraoperative imaging can be obtained when performing IORT, easing the applicator positioning and resulting in a more precise target irradiation. Operating times would be minimally extended with this procedure. A clinical study will initiate based on these findings.