Towards clinical application: Potential margin reduction in proton therapy with prompt-gamma imaging
Stefanie Bertschi,
Germany
PO-1848
Abstract
Towards clinical application: Potential margin reduction in proton therapy with prompt-gamma imaging
Authors: Stefanie Bertschi1, Jonathan Berthold1,2, Julian Pietsch1,2, Julien Smeets3, Guillaume Janssens3, Kristin Stützer1,2, Christian Richter1,2,4,5
1OncoRay – National Center for Radiation Research in Oncology, Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, Helmholtz-Zentrum Dresden - Rossendorf, Dresden, Germany; 2Helmholtz-Zentrum Dresden - Rossendorf, Institute of Radiooncology - OncoRay, Dresden, Germany; 3Ion Beam Applications SA, Research, Louvain-la-Neuve, Belgium; 4Department of Radiotherapy and Radiation Oncology, Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany; 5German Cancer Consortium (DKTK), Partner Site Dresden, Germany and German Cancer Research Center (DKFZ), Heidelberg, Germany
Show Affiliations
Hide Affiliations
Purpose or Objective
In proton therapy (PT), considerable clinical planning margins around the target are needed to account for various uncertainties. We provide the first estimation of their potential reduction when using prompt gamma imaging (PGI) for routine treatment verification and intervention in prostate cancer PT.
Material and Methods
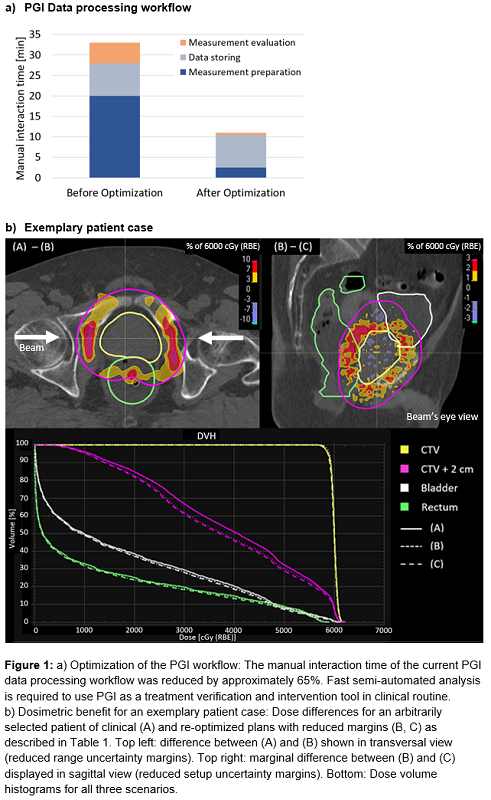
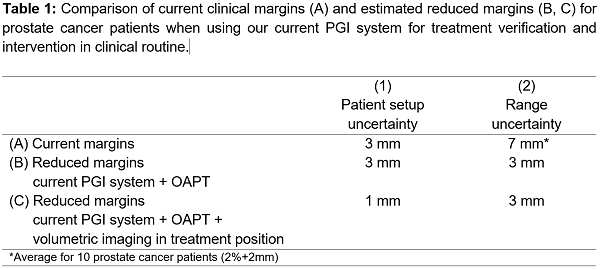
Three scenarios were investigated based on clinical PGI data of 10 prostate cancer patients treated with hypofractionated (3Gy/Fx) PBS (74 fractions/148 fields monitored). Scenario A describes the current clinically used margins during CTV-based robust treatment planning for (1) patient setup uncertainties and (2) dual-energy CT based range uncertainties of 2%+2mm. Scenario B estimates the potential margin reduction when using the current 2nd generation PGI system as trigger for an online adaptive proton therapy (OAPT) workflow. Hereby, a setup protocol using orthogonal X-ray imaging, immediate PGI analysis and, if necessary, online re-planning based on volumetric imaging, were assumed. To quantify the margin reduction potential, the accuracy of the current PGI system for a field-wise evaluation was estimated, considering only the statistical fluctuation (2σ) of the PGI information per field since the systematic uncertainty was previously shown to be negligible. In-room CTs in treatment position, available for all 74 fractions, were used to calculate the PGI ground-truth. Furthermore, the current PGI data processing workflow was optimized to enable a semi-automated analysis (Fig. 1a). Scenario C describes further margin reduction for an OAPT workflow including initial volumetric imaging at isocenter and adaptation before irradiation. For an exemplary patient case, the benefit of the reduced margins was investigated by comparing the dose distributions of the clinical plan and the re-optimized plans with reduced margins.
Results
Compared to scenario A (current clinical situation), scenario B (range verification with current PGI system to trigger OAPT) reduces the current range uncertainty margins, which are already considerably smaller than commonly used margins based on single-energy CTs, by 57% to 3mm while maintaining setup uncertainty margins. In scenario C (OAPT workflow with volumetric imaging and adaptation before irradiation), also the setup uncertainty margins are reduced by 66% to 1mm (Tab. 1). In the exemplary patient case, reduced range uncertainty and reduced setup uncertainty margins resulted in locally reduced dose to surrounding tissue of 10% and 3%, respectively (Fig. 1b).
Conclusion
Substantially reduced planning margins are feasible for the investigated treatment region when using PGI for treatment verification and intervention in clinical routine - resulting in a considerable dosimetric benefit. PGI acts as an important enabler for closed OAPT workflows not only due to the improved treatment accuracy as shown here, but also by providing an independent QA measure on patient level for the online-adapted plan.