The effect of PTV density on the quality of lung plans in a 1.5 T magnetic field
Frank Brewster,
United Kingdom
PO-1827
Abstract
The effect of PTV density on the quality of lung plans in a 1.5 T magnetic field
Authors: Frank Brewster1, Jack Doherty2, Linnéa Freear1, Robert Chuter1,3
1The Christie NHS Foundation Trust, Christie Medical Physics and Engineering, Manchester, United Kingdom; 2The University of Manchester, Faculty of Biology, Medicine and Health, Manchester, United Kingdom; 3The University of Manchester, School of Cancer Sciences, Manchester, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
The Elekta Unity MRL (Elekta AB, Stockholm) combines a 7 MV linac with a 1.5 T MR scanner, allowing for daily imaging and online plan adaptation with improved soft tissue contrast. Lung tumours can exhibit large inter and intra-fraction anatomical changes. As such, there is a desire to investigate if the MRL may be able to counteract these effects.
Due to the magnetic field, secondary electrons are subject to the electron return effect (ERE). This is of particular concern in lung cancer due to the low-density tissue interfaces and can cause a build-up of dose in the chest wall as well as a reduction in dose at the target.
This project aimed to determine if there was a correlation between PTV relative electron density (rED) and plan quality and set a lower limit on PTV density if there was.
Material and Methods
13 patients were selected from patients used during commissioning, previously treated on our MRL or had been treated on a conventional linac at our centre. All patients had been planned on the average scan of a 4DCT with motion-adapted GTVs. Plans were made using Monaco research version 5.19.05 (Elekta AB, Stockholm) to a prescription of 55 Gy in 20#. The planning solution used was the same as used clinically; 21 equi-spaced IMRT beams, with any entering through the spinal cord or contralateral lung removed. All plans were rescaled to give a mean ITV dose of 55 Gy.
Plans were then re-optimised with the magnetic field turned off and clinical goal dose statistics were extracted from both plans. A chest wall contour was made by creating a 1 cm margin around the lung boundary and subtracting the target.
Results
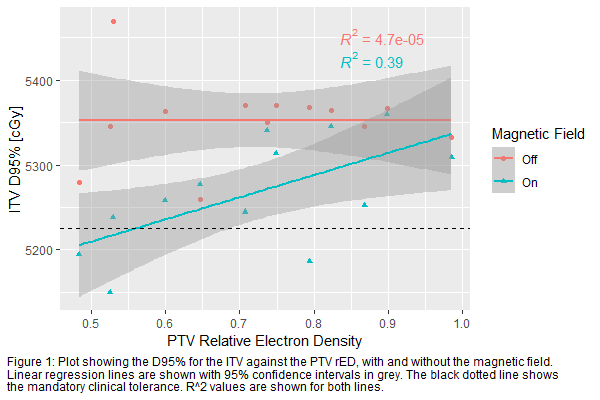
All dosimetric criteria were met for 10 out of 13 patients. In the remaining 3 plans, all dosimetric criteria came into tolerance once the magnetic field was switched off. Figure 1 shows the ITV D95% for all plans. This shows moderate correlation with PTV rED when the magnetic field is on. It also shows that there is a drop in coverage for all patients except one with the magnetic field on. This plan was investigated, and it was found to be due to the target being exceptionally bulky and close to the mediastinum, causing the ERE to improve coverage. Correlation was seen between the ITV D1cc and PTV rED (R^2=0.2), however; this was weak and differences in fit lines were within 95% confidence intervals.
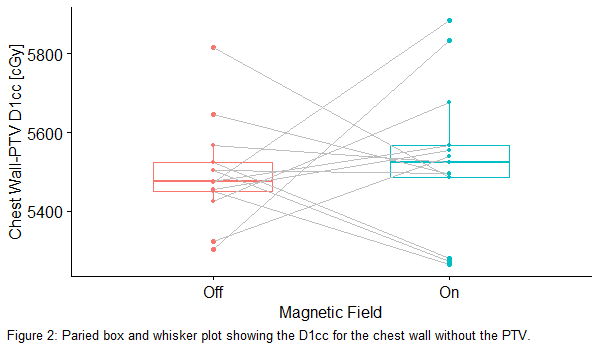
There was no correlation seen between PTV rED and chest wall dose. Although hot spots were seen in the chest wall for some patients, there was no significant difference in the chest wall D1cc between plans with the magnetic field on and off, as seen in Figure 2.
Conclusion
This study has shown that there is moderate correlation between coverage and PTV rED in a magnetic field and that coverage can be improved when no magnetic field is present. As such, it is unlikely to be possible to produce acceptable plans for patients with a PTV rED≲0.6 due to either not meeting tolerances or there being a >2% drop in coverage.