Feasibility of Xoft Axxent Electronic IORT for intracranial tumors in terms of radiation dosimetry
PO-1817
Abstract
Feasibility of Xoft Axxent Electronic IORT for intracranial tumors in terms of radiation dosimetry
Authors: Sumeyra Can1, Didem Karaçetin1, Pierfrancesco Silli2, Cristian Perez3, Özge Atilla1, İlknur Harmankaya1
1Basaksehir Cam and Sakura City Hospital, Radiation Oncology, Istanbul, Turkey; 2Xoft Inc., A Subsidiary of iCad. Inc., Business Development, Florence, Italy; 3Xoft Inc., a Subsidiary of iCad. Inc., Business Development, Madrid, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
The study aimed to analyze IORT plans utilized with Xoft Axxent eBx which is a 50 kVp low energy IORT system comparing it with non-coplanar VMAT SRS treatment technique using Elekta Versa HD™ in terms of radiation dosimetry for single target high grade primary CNS tumors and intracranial metastatic disease. The patients who have non-operated tumor and treated with SRS were considered, however, it was aimed to show the benefit of IORT might present even better advantages to protect OAR’s and to reduce possible radiation necrosis.
Material and Methods
CT images were acquired with a 1.0 mm slice thickness and fused with a T1 weighted gradient-echo MRI sequence with contrast media for target delineation. Non-coplanar VMAT plans were devised in the Monaco® TPS and all patients were treated with VMAT SRS. The treatment plan prescription was 20 Gy in single fraction to PTV with the coverage rate of 95%. All CT data sets were imported to BrachyCare TPS to visualize the dose distribution of IORT plans to deliver 20 Gy at the applicator surface. PTV was assumed as the resection cavity which is filled spherical balloon applicator volume at the time of surgery. Gradient index (GI) which was calculated based on Paddick formula and NTCP values calculated based on Lyman-Kutcher-Burman method.
Results
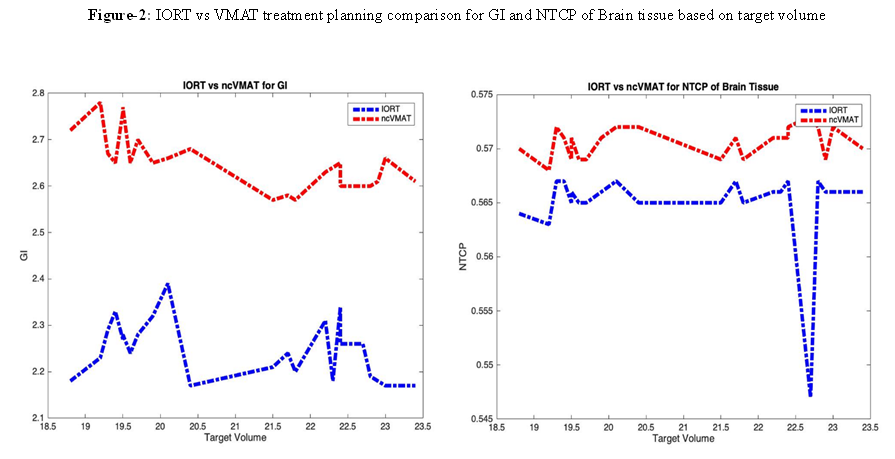
The 23 patients were retrospectively analyzed. The mean Dmax of Brainstem was (4.43 ± 3.13) Gy in VMAT plans, and it was (3.27 ± 2.80) Gy in IORT plans. IORT has great advantageous to reduce dose even if the tumor location is close to critical structures. IORT dose was approximately 65% and 68% less than VMAT dose for eyes and optic nerves respectively. Additionally, V2Gy, V10Gy, V12Gy of Brain-PTV were also analyzed for radiation necrosis. IORT was crucial to provide better V2Gy result for Brain-PTV due to the nature of source energy. However, VMAT plan was superior to control high dose region outside of PTV. Dose distribution in both approaches was shown in Figure-1. The GI value was 2.65 and 2.24 in VMAT plan and IORT respectively. IORT was superior to provide low-dose spillage. In both approaches, NTCP value meet the criterion which is ≤1.0, however, IORT (mean NTCP ≈ 0.555) is superior to VMAT (mean NTCP ≈ 0.575) for NTCP results as expected. IORT and VMAT plan comparison for GI and NTCP results was shown in Figure-2.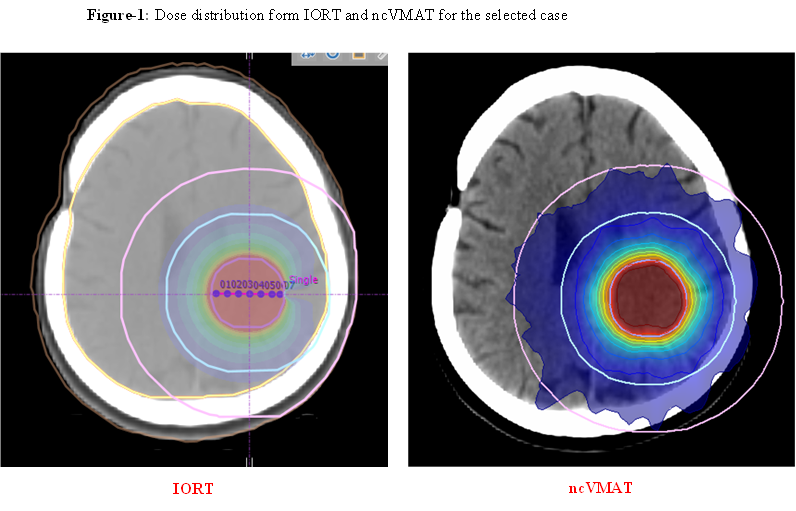
Conclusion
Xoft Axxent eBX system is better to reduce OARs dose and it is superior to VMAT plan especially when the target has close proximity to critical structures. Moreover, low energy IORT system provides better control in low dose region at outside of the target and it results better GI which it is indicating greater dose falloff and better dose conformity. As a result, the unique dosimetry of IORT has potential to increase radiobiological advantages in achieving local control of single target brain tumors. However, detailed investigation in conjunction with radiation necrosis and novel systemic treatments after surgery is crucial.