Dosimetric characteristics of an in-house developed collimator for preclinical minibeam radiotherapy
PO-1785
Abstract
Dosimetric characteristics of an in-house developed collimator for preclinical minibeam radiotherapy
Authors: Canan Koksal Akbas1,2, Sara Broggi3, Cesare Cozzarini4, Nadia Di Muzio4, Francesco Cavaliere5, Paolo Milani5, Antonella Del Vecchio3, Claudio Fiorino3, Carlo Tacchetti1, Antonello Spinelli1
1San Raffaele Scientific Institute, Experimental Imaging Center, Milan, Italy; 2Istanbul University Oncology Institute, Medical Physics Department, Istanbul, Turkey; 3San Raffaele Scientific Institute, Medical Physics Department, Milan, Italy; 4San Raffaele Scientific Institute, Radiotherapy Department, Milan, Italy; 5Università degli Studi di Milano, Department of Physics, Milan, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Preclinical studies have indicated that minibeam radiotherapy (MBRT), is one of the spatially fractionated techniques that can enhance the therapeutic index. In order to obtain reliable results from radiobiological experiments using MBRT, accurate dosimetry is an essential requirement. The purpose of this current study is to investigate the dosimetric characteristics of an in-house developed minibeam collimator (MBC) for preclinical MBRT.
Material and Methods
A small animal irradiator (SmART, PXI), available at the San Raffaele Scientific Institute Preclinical Imaging Facility was used as an X-ray source (225 KV, 13 mA): a collimator made of lead (40x40 and 5 mm thickness) was built to generate minibeams. Absolute dosimetry for the unmodulated beam was performed using a farmer-type ion chamber following the AAPM TG-61 protocol and Radiochromic EBT3 (GC) films scanned at 800 dpi were used for relative dosimetry of minibeams. The output factor (OF) was calculated as the ratio of the dose measured by calibrated GC irradiated with MBC with respect to the open field at the phantom surface. The peak-valley-dose-ratio (PVDR), beam (FWHM), and distance between peaks were assessed using GC films. The depth dose (DD) measurement of MBC was performed by placing GC films between PMMA slabs, with a 2.5 mm thickness each. The dependence of the PVDR and FWHM with depth was determined from the DD measurement.
Results
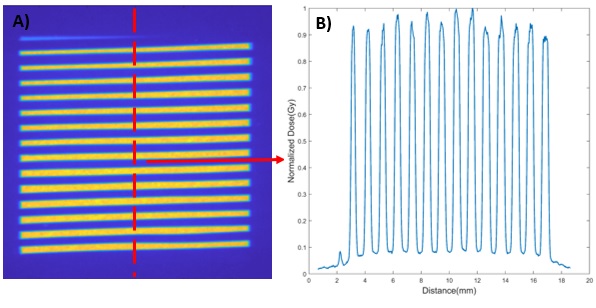
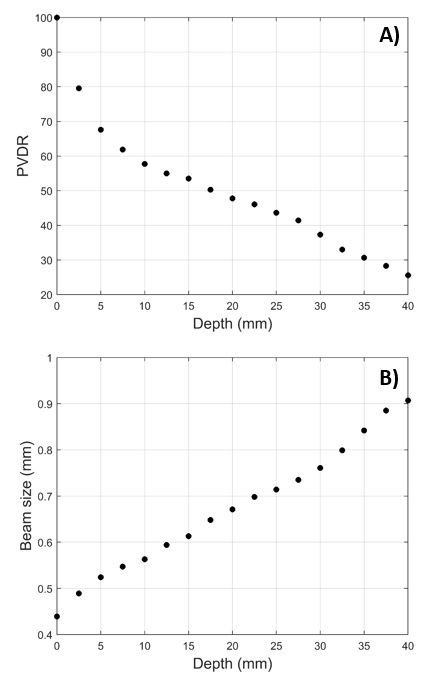
The dose distributions and lateral dose profile of minibeams measured by EBT3 at the PMMA phantom surface are shown in Figure 1-A and Figure 1-B, respectively. It has been seen that the variation of the peak values along the profile was approximately 10%. The valley values were homogenous. The OF, PVDR, FWHM, and distance between peaks were found to be 0.910±0.019, 11.58±0.20, 0.439±0.022 mm, and 1.098±0.048 mm, respectively. The PVDR decreases exponentially with depth (Figure 2-A). The FWHM increases up to 0.907 mm at 40 mm of depth because of the beam divergence (Figure 2-B).
Conclusion
In this preliminary study, dosimetric characterization of an in-house developed minibeam collimator for preclinical MBRT could be accomplished using ion chamber in combination with GC films, adapting methodologies in use for small field dosimetry in external radiotherapy.