Evaluation of block thickness for smaller lungs at extended SSD treatment technique in TBI
PO-2016
Abstract
Evaluation of block thickness for smaller lungs at extended SSD treatment technique in TBI
Authors: Raju Srivastava1, Olteanu Ana Maria Luiza1, Frederik Vanhoutte1
1Gent University Hospital, Radiation Oncology, Gent, Belgium
Show Affiliations
Hide Affiliations
Purpose or Objective
Total body irradiation (TBI) is used to treat a range of malignant diseases in both adult and pediatric patients. Its practice varies worldwide with radiotherapy centers and there are multiple techniques to deliver TBI. The aim of this study was to investigate the calculated and measured block thickness transmission in our center and the applicability of the calculations for patients with smaller lungs.
Material and Methods
The study involved ten TBI treatments. The patient is treated in standing position to reduce the dose. Patients are treated in AP/PA orientations at extended source to skin distance (SSD) at 4 meter. The gantry angle is set to 86°, maximum field (40 x 40 cm2 at isocenter) at 45° collimator. A 18 MV is used to treat the patient on our twinned Elekta Synergy® accelerators, with a 2 cm acrylic spoiler to reduce the skin-sparing effect. The measurements are use in in-house made software to calculate the expected mid-thorax dose and the lung block thickness for the desired block transmission. Four (Rt ant and pots / Lt ant/post) HVL lung blocks are made out of epsi metal 96 (52.5% Bi, 32.0% Pb, 15.5% Sn). The thickness of the blocks (x) is calculated using the usual formula for narrow-beam geometry.

Before start of treatment, the transmission of the lung blocks is measured in a homogenous phantom at patient specific mid-lung depth. In TBI the field is many times larger than the block and the narrow beam conditions at the block center are not met if the block dimensions. Become comparable to the scatter range. The above equation is adapted for smaller lung to approximate the scatter contribution sf (sf>1.0) from large field at extended SSD.
We express the scatter contribution as a virtual reduction of the block thickness t. This value needs to be added to the calculated block thickness to reach the desired attenuation in patients with smaller lung sizes.
Results
Figure 1 displays the calculated and measured transmission of the lung blocks. For this study , the transmission is measured in solid water phantom at 10 cm homogeneous backscattered thickness and exact depth of anterior thorax wall using a PTW 0.6cc ion chamber. The average block transmission is 72% of block thickness 0.85 cm. The maximum deviation accepted in our department is ± 2% . However, for the smallest lung blocks we made so far, 24% and 10% smaller in length and breadth respectively from average lung blocks, the deviation exceeded our criteria. The result was not added to the figure 1. The lung blocks has been re-made by adding 1mm additional thickness and subsequently passed our criteria.
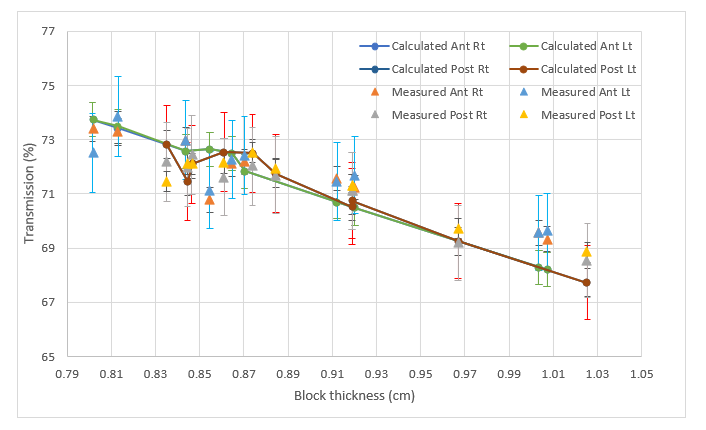
Figure1. Calculated and measured lung block thickness transmission. The error bar shows ± 2% tolerance criteria.
Conclusion
The study presents the effect of simplified block thickness calculation for TBI in our department. Small lungs blocks need 0.1cm additional thickness on calculated thickness due to the scatter component from large field at extended SSD treatment.