A new and practical approach to dose constraints in re-irradiation.
PO-1992
Abstract
A new and practical approach to dose constraints in re-irradiation.
Authors: Sandra Vieira1, Joep Stroom1, Ana Soares2, Carlo Greco1
1Champalimaud Foundation, Radiotherapy, Lisbon, Portugal; 2Mercurius Health, Radiotherapy, Lisbon, Portugal
Show Affiliations
Hide Affiliations
Purpose or Objective
Re-irradiation has become more frequent, complex, and is not only palliative anymore. Different fractionation schemes are used making dose comparisons challenging, especially since 3D fraction-dose conversions are usually not commercially available. Furthermore, organ at risk (OAR) repair factors and validated dose constraints are still lacking. To start bringing some consistency to dose constraints for re-irradiations, we propose a simple method based on summation of relative values, independent of the fractionation scheme or constraint type used.
Material and Methods
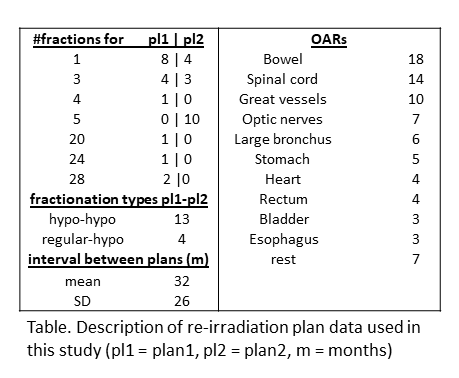
We considered 16 patients re-irradiated with different fractionations (f1 and f2) and in total 66 relevant OARs. Data selection was based on the variety of OARs and fractionation schemes (see Table). In our proposed percentage method (PM), the planned DVH dose at Vconst (i.e. Dplan(Vconst)) is determined, and subsequently divided by the constraint dose (i.e. Dconst(Vconst)) for both plans for each OAR. These relative ratios (RR) are then summed (RR1+RR2) and should be <= 100%. The relativity implies that constraints do not need to have the same Vconst enabling the combination of hypo- and regular-constraints.
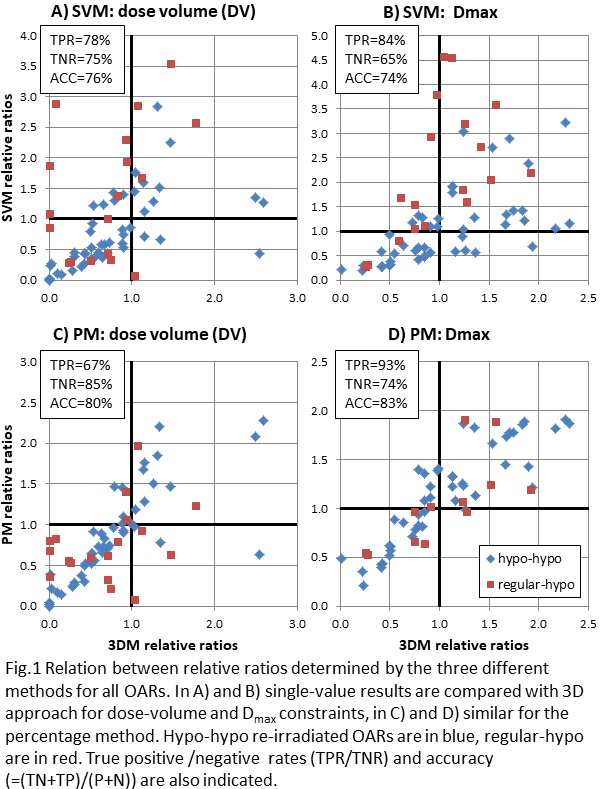
We compared the PM with two different strategies: a 3D and a single-value approach. Firstly, the 3D method (3DM) uses a home-written Varian Eclipse script and the LQ model to convert 3D doses from plan1 to the fractionation of plan2 (f2), after which rigid registration and dose summation yields the total dose. Total OAR doses are then evaluated using the constraints for f2. Secondly, the single-value method (SVM), which is more widely used, takes the sum of single critical dose values from each fractionation scheme, after an LQ conversion of the single dose value of plan1 to f2.
For each OAR and constraint type, we plotted the RR per method and we calculated the true positive/negative rates and accuracy of the PM and SVM. For now, we ignored OAR repair in between treatments, only considered single re-irradiations, and assumed alpha/beta=3 for all OARs.
Results
In Fig 1 the relation between critical OAR doses for the different methods is depicted, showing that largest differences occur in regular-hypo re-irradiations. The PM is at least as good at predicting the 3D results as the SVM. This is confirmed by the calculation of the accuracy which is 76% and 74% for DV and Dmax constraints of the SVM, respectively, and 80% and 83% for the PM. Further advantages of the PM are that plans are evaluated by their validated constraints and no image/dose registration or LQ conversion schemes are required. However, there is no radiobiological justification as yet.
Conclusion
Our preliminary results indicate that relative dose constraints are a simple, practical, and generally-applicable tool to evaluate and determine re-irradiation OAR doses. Its accuracy is comparable with existing practices and the tool may also be applied to plans with different fractionation schemes delivered during the same treatment.