Implementation of a tangential IMRT solution for breast cancer in Monaco TPS
PO-2054
Abstract
Implementation of a tangential IMRT solution for breast cancer in Monaco TPS
Authors: Sara Poeta1, Diana Rodriguez Garcia2, Younes Jourani1, Antoine Desmet3, Nick Reynaert2
1Institut Jules Bordet, Medical Physics , Brussels, Belgium; 2Institut Jules Bordet, Medical Physics, Brussels, Belgium; 3Institut Jules Bordet, Radiation Oncology, Brussels, Belgium
Show Affiliations
Hide Affiliations
Purpose or Objective
The aim of this work was to implement an efficient tangential solution for breast cancer treatment based on dynamic multi-leaf collimator (dMLC) inverse planning in Monaco TPS (v6.0, Elekta AB, Stockholm, Sweden) while preserving the organs at risk (OAR) constraints based on conformal 3D solutions.
Material and Methods
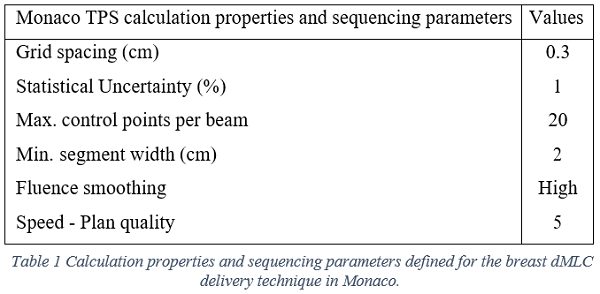
Twenty-eight consecutive patients treated were selected: 15 left (LBC) and 13 right (RBC) breast cancers, respectively. Contouring was performed according to ESTRO guidelines. All LBC patients were treated with breath hold technique. The dMLC technique was based on inverse planning in Monaco with 6MV photons. This technique consisted on two opposed tangential beams, as set for conformal 3D techniques, with collimators adapted to be parallel to the chestwall with specific parameters in Monaco to mimic the use of wedge or field in field technique. The main calculation properties and sequencing parameters of the plans are described in table 1.
The prescribed dose was 40,05Gy in 15 fractions to the PTV Breast (breast or thoracic wall). Indications of lymph node irradiation were excluded. All plans were normalized to the 95% of the prescribed dose covering 95% of the PTV Breast. Doses to OAR were evaluated against our in-house constraints and two well-known protocols: DBCG HYPO trial and RTOG 1005. The LINAC output was measured to evaluate deliverability and quality of the plans based on the gamma index tool.
Results
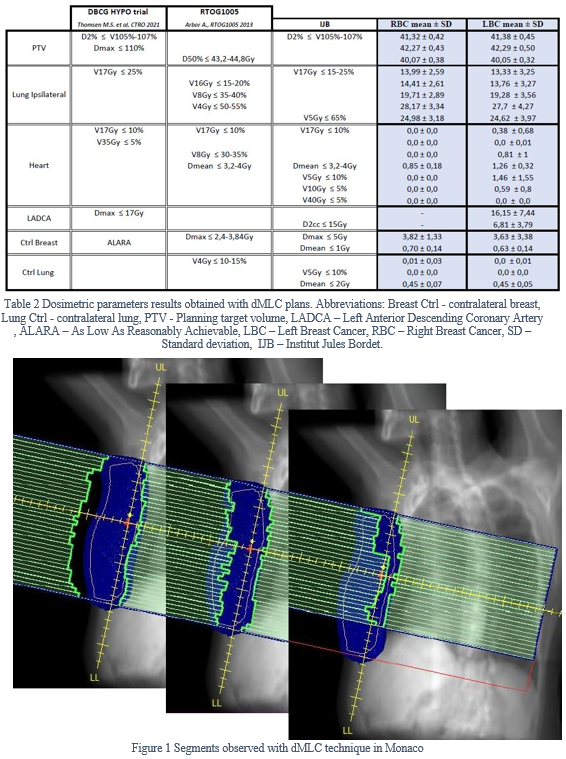
Table 2 shows the dosimetric parameters obtained with dMLC technique compared with the three constraint protocols: DBCG HYPO trial, RTOG1005 and in-house constraints. The results were separated between left and right breast cancer patients.
Most results were under the constraints required from any of the protocols. For LADCA, 5 patients out of 15 received more than 17Gy in maximum dose. However, D2cc < 15Gy was achieved for all the patients. The mean conformity index achieved was 0.75 ± 0.07. The mean monitor units per plan was about 290±40. The large segments sizes encompassing the entire breast height are visible in figure 1.
Regarding the QA measurements, all plans passed the 3%/3mm gamma index criteria.
Conclusion
The main objectives of this work were achieved. The parameters defined in table 1 limited considerably the plan modulation and thus ensuring a fast and robust treatment delivery. This is particularly visible in the low number of monitor units (290 ± 40) and in the large segments sizes.
Regarding the constraints achieved whether they were suitable or not, based on published literature (Thomsen M.S. et al, CTRO 2021; Arbor A. et al, RTOG1005 2013; Piroth M.D. et al, Strahlenther Onkol 2019; Fogliata A. et al, IJROBP 2017; Koivumäcki T. et al, R&O 2016; Marrazzo L. et al, Physica Medica 2022), we believe this technique offers good dosimetric results.
In conclusion, dMLC technique with specific parameters in Monaco is an optimal technique for whole breast irradiation.