Assessment of the GE Metal Artifact Reduction option in CTs used for dose calculations with Eclipse
Stefania Linsalata,
Italy
PO-2053
Abstract
Assessment of the GE Metal Artifact Reduction option in CTs used for dose calculations with Eclipse
Authors: Stefania Linsalata1, Rita Borgheresi2
1Azienda Ospedaliera Universitaria Pisana, Medical Physics Unit, Pisa, Italy; 2Azienda Ospedaliera Universitaria Senese, Medical Physics Unit, Siena, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
To assess the impact of the GE Metal Artifact Reduction (MAR) option on dose calculation accuracy for the Acuros XB (AXB) and Analytical Anisotropic Algorithm (AAA) Varian photon algorithms.
Material and Methods
A CIRS 062MA Electron Density phantom with high density optional insert was imaged in a GE DiscoveryRT CT simulator with and without the MAR option to obtain two HU-to-density correction tables. A slab PMMA phantom (44x11x16 cm^3 and density 1.183 g/cm^3) with a removable insert of titanium (22x2x2 cm^3 and density 4.506 g/cm^3) was imaged with the two same imaging protocols. Dose calculations in these two slab phantom CTs were done after the application of the proper HU-to-density curve. Due to AXB calculation properties (i.e., the upper limit density of 3 g/cm^3 for the use of the HU-to-density automatic conversion) the exact volume of the titanium insert was overridden with the HU corresponding to the real insert density, namely HU=5611 with MAR and HU=6343 without MAR. No override was necessary for the AAA algorithm.
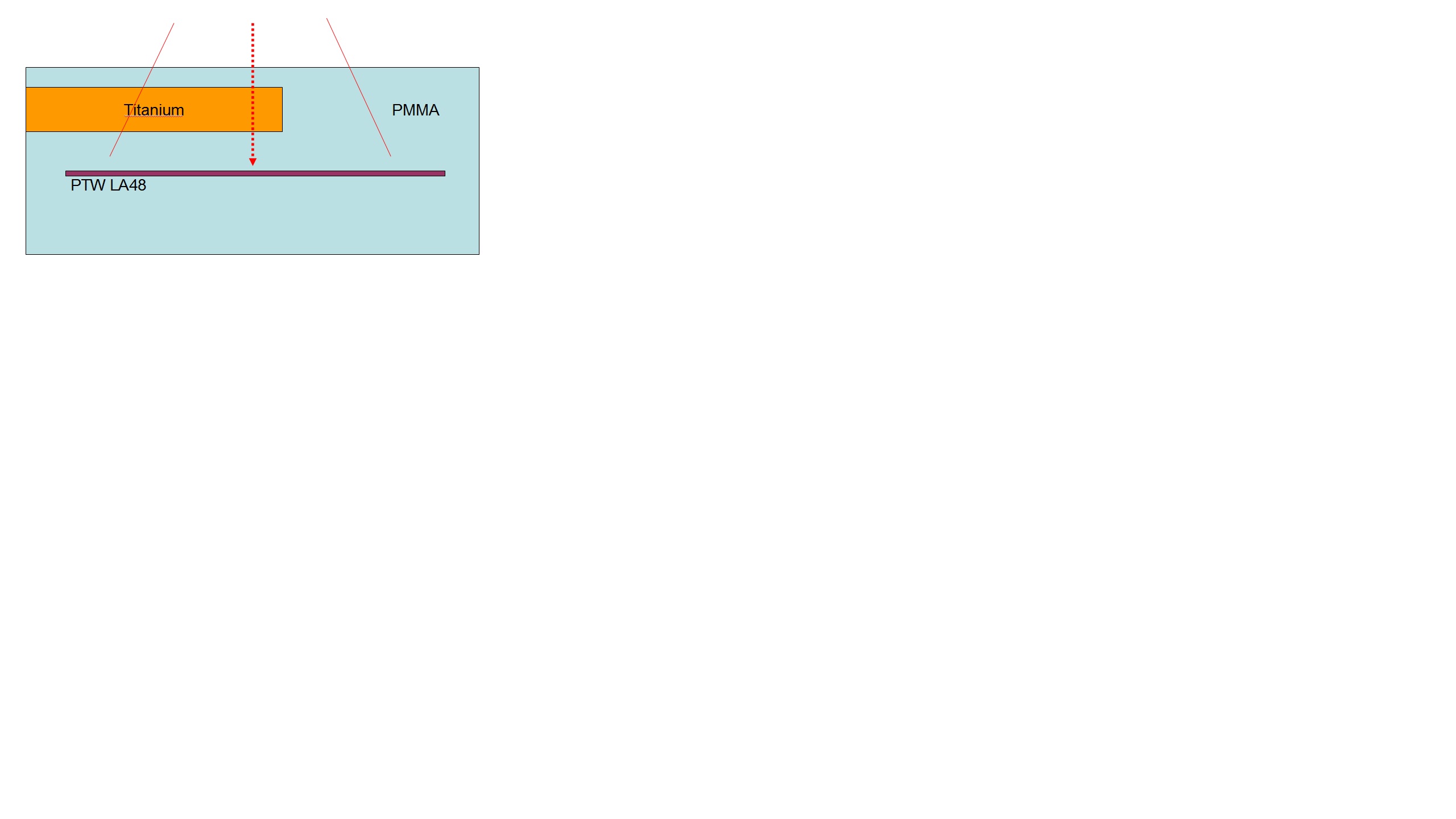
Absorbed dose profiles at 5 cm depth and SSD=95cm of a 10x15 cm^2 Varian Clinac DHX open field of 6 MV and 15 MV were calculated with the AXB and AAA algorithms in the TPS Varian Eclipse v. 16.1. Dose calculations, reported as dose-to-water, were compared with measured profiles, obtained with a PTW LA48 linear ionization chamber array, positioned in the slab PMMA phantom to reproduce exactly the calculated fields. The detector was previously cross-calibrated in dose-to-water against a Farmer ionization chamber for the two considered beam qualities. A schematic view of the setup is reported in Figure.
Results
The percentage difference between measured and calculated doses in two off-axis points, namely - 4 cm and + 4 cm from the isocenter in the longitudinal direction, corresponding at points downward titanium and PMMA respectively, were reported in Table. The average accuracy of the dose profiles for 6 and 15 MV respectively was for AAA and MAR -3.8% and -4.0%; for AAA without MAR -1.7% and -2.8%; for AXB and MAR -2.3% and -2.0% and for AXB without MAR -1.4% and -1.7%.
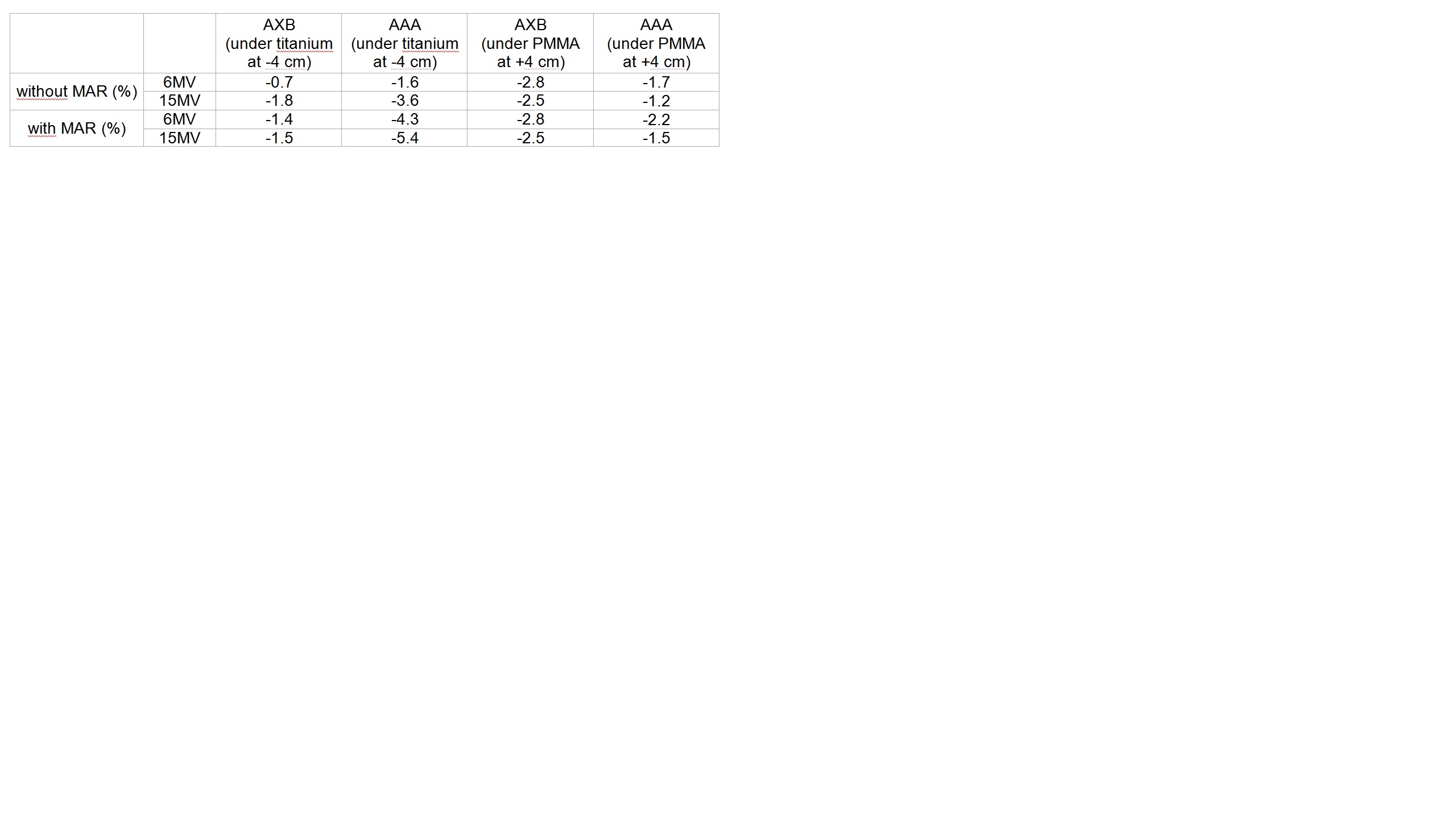
Conclusion
Our results show that, limited to the reported materials and irradiation conditions, the MAR option embedded in the GE CT scanners should be used carefully in combination with the AAA calculation algorithm, meanwhile has limited impact on AXB calculations, probably due to the property of the latter of limiting the HU-to-density automatic conversion for the higher density. Although more realistic situations should be investigated, such as real prosthesis or dental implant, our results suggest that the wide use of the MAR option in planning CT images, thanks to the increased image quality, seems justified for dose calculation with AXB but should be carefully considered with AAA.