Plan quality & deliverability of IMRT plans for lung cancer using various leaf motion calculators
Eva Y. KONG,
China, Hong Kong Special Administrative Region
PO-2042
Abstract
Plan quality & deliverability of IMRT plans for lung cancer using various leaf motion calculators
Authors: Eva Kong1, Nelson T.C. Fung1, Michael C.H. Lee1
1Pamela Youde Nethersole Eastern Hospital, Medical Physics Department, Hong Kong, Hong Kong (SAR) China
Show Affiliations
Hide Affiliations
Purpose or Objective
To evaluate whether plan qualities and delivery accuracies of IMRT plans for lung tumors could be affected by the choice of leaf motion calculator (LMC) algorithms.
Material and Methods
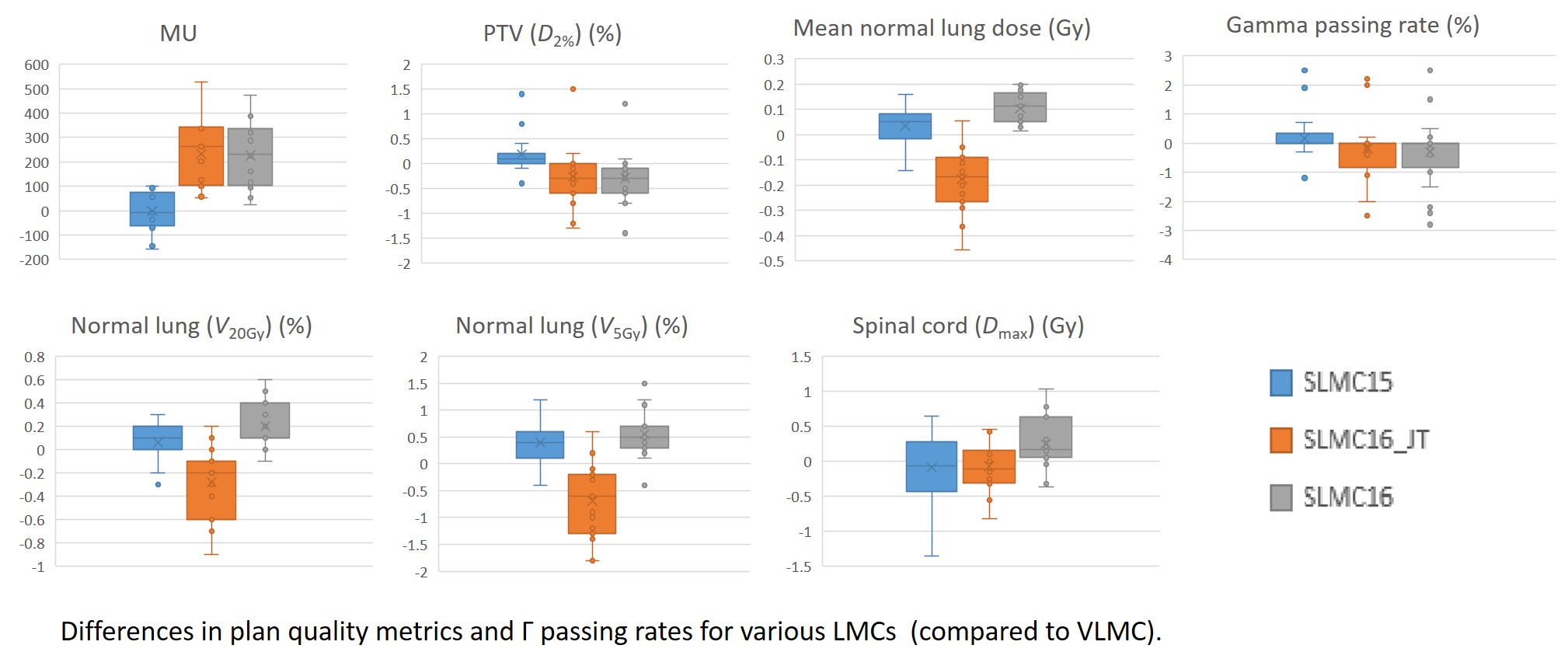
A total of 15 conventional fractionated lung cases were studied. For each case, 4 plans were optimized with the same beam arrangement, dose-volume objectives and number of iterations but different LMC algorithms were used, namely: 1. Varian LMC 16.1.0 (VLMC), 2. Smart LMC 15.5.11 (SLMC15), 3. Smart LMC 16.1.0 with and 4. without jaw tracking (SLMC16_JT and SLMC16). All plans used the sliding window technique with 6MV photon beams. Dose calculation were performed using AcurosXB 16.1.0 with intermediate dose taken into account. To facilitate the comparison of plan quality metrics, SLMC15, SLMC16 and SLMC16_JT plans were normalized such that the PTV (D98%) were identical to those in the VLMC plan. Delivery accuracies of the plans in Varian TrueBeamTM were assessed by measurements using the Delta4 phantom+ and Γ analysis was used to compare the planned and delivered dose with the criteria of 3%/2mm. The differences (with respect to the VLMC plan) in PTV (D2%), normal lung (NL) (V5Gy, V20Gy, mean dose), spinal cord (SC) (Dmax), total monitor units (MU) and Γ passing rates were evaluated using paired student’s t-tests, with p<0.05 considered as statistically significant.
Results
Significant differences in MU were observed in both SLMC16 and SLMC16_JT plans, with a mean increase of 225.9 MU and 232.8 MU respectively. Statistically, SLMC16_JT plans showed superior normal lung sparing while sparing of both the lung and the spinal cord were worse for SLMC16 plans; SLMC15 plans were comparable to the VLMC plans in terms of OAR sparing except in the normal lung V5Gy. Although statistical significances were detected in some dose-volume parameters in critical organs, it should be noted that the actual differences were generally small and may not be clinically meaningful. Differences in PTV hotspots and Γ passing rates were not significant across all LMC plans. Compared with VLMC, both versions of SLMC did not show obvious advantages in radiotherapy planning for lung tumors clinically. Slightly better OAR sparing could be achieved using jaw tracking, yet it could induce a higher MU which may increase treatment time and leakage dose to patients.
Mean differences (p) w.r.t. the VLMC plan
| MU
| PTV (D2%) (%)
| NL V5Gy (%)
| NL V20Gy (%)
| Mean NL dose (Gy)
| SC Dmax (Gy)
| Γ passing rate (%)
|
SLMC15
| -2.2
(0.93)
| 0.2
(0.11)
| 0.4
(0.003)
| 0.1
(0.19)
| 0.0 (0.11)
| -0.1 (0.51)
| 0.2 (0.38)
|
SLMC16
| 225.9
(<0.001)
| -0.3
(0.06)
| 0.6 (<0.001)
| 0.2
(0.002)
| 0.1 (<0.001)
| 0.2 (0.03)
| -0.3 (0.29)
|
SLMC16_JT
| 232.8 (<0.001)
| -0.3
(0.13)
| -0.7
(0.003)
| -0.3
(0.004)
| -0.2 (<0.001)
| -0.1 (0.46)
| -0.2 (0.44)
|
+ve indicates a lower value in the VLMC plan.
Conclusion
Although delivery accuracy was unaffected by the choice of LMCs, plan qualities including OAR doses, particularly the total number of MU, could be influenced by the LMC types (Varian/Smart), techniques (with/without jaw tracking) or even the versions (15/16).