Multiparametric MRI and PET to predict ISUP grade groups in prostate cancer patients
PO-2124
Abstract
Multiparametric MRI and PET to predict ISUP grade groups in prostate cancer patients
Authors: Erik Nilsson1, Kristina Sandgren1, Josefine Grefve1, Joakim Jonsson1, Jan Axelsson1, Angsana Keeratijarut Lindberg1, Karin Söderkvist2, Camilla Thellenberg Karlsson2, Anders Widmark2, Lennart Blomqvist3, Sara Strandberg4, Katrine Riklund4, Anders Bergh4, Tufve Nyholm1
1Umea University, Department of Radiation Sciences, Radiation Physics, Umea, Sweden; 2Umea University, Department of Radiation Sciences, Oncology, Umea, Sweden; 3Karolinska Institute, Department of Molecular Medicine and Surgery, Solna, Sweden; 4Umea University, Department of Radiation Sciences, Diagnostic Radiology, Umea, Sweden
Show Affiliations
Hide Affiliations
Purpose or Objective
To investigate the potential of multiparametric magnetic resonance imaging (mpMRI) and positron emission tomography (PET) for prostate cancer (PCa) risk stratification, using whole-mount registered histopathology as reference standard.
Material and Methods
Fifty-five men planned for radical prostatectomy with elevated prostate-specific antigen and biopsy-proven PCa were included in this study. [⁶⁸Ga]PSMA-11 PET/mpMRI and [¹¹C]Acetate PET/CT were performed prior to surgery. Prostate glands were delineated on T2-weighted (T2w) images and a mould was 3D-printed for each patient. Resected prostate specimens were placed inside their shape-preserving moulds for ex-vivo T2w imaging, followed by histopathological preparation and subsequent evaluation. The evaluation resulted in digital annotations showing the location of lesions and their International Society of Urological Pathology (ISUP) grade groups (IGG). The in-vivo T2w images served as a common frame of reference for all image data. The histopathology was first registered to the ex-vivo T2w, which in turn was co-registered to the in-vivo T2w. We used PET and mpMRI data to differentiate between ISUP grades in two cases: IGG 3 vs. IGG 2 and IGG ≥ 3 vs. IGG ≤ 2. PET uptake was quantified in maximum standardized uptake values (SUVmax). mpMRI was quantified in relative measures of the maximum volume transfer constant (RKtrans), median apparent diffusion coefficient (RADC) and the median intensity of T2w images (RT2w). The superscript R signifies that these values were normalized to the corresponding mean intensities of healthy prostatic tissue. The performance was evaluated by receiver operating characteristics (ROC) analysis, using a fast implementation of Delong’s algorithm to compare the area under the ROC curves (AUCs).
Results
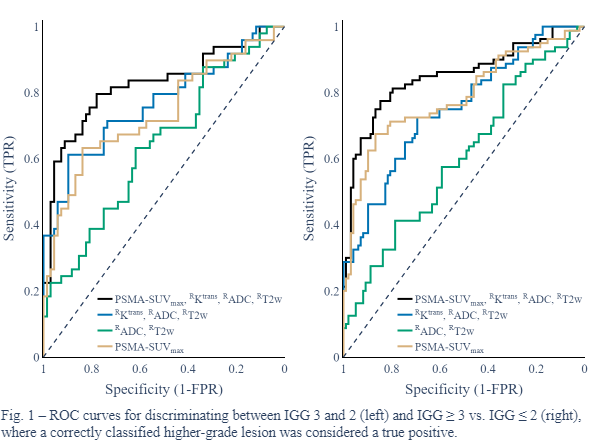
We identified 660 lesions in total. The results are based on the 178 lesions having an in-plane area larger than a circle with a radius roughly equal to the upper limit of the estimated uncertainty of the registration method (≥ 20 mm²). Cut-off values for PSMA-SUVmax combined with Acetate-SUVmax, RKtrans and RADC yielded AUCs of 0.88 for IGG 3 vs. IGG 2 and 0.89 for IGG ≥ 3 vs. IGG ≤ 2. PSMA-SUVmax alone achieved an AUC of 0.73 for IGG 3 vs. IGG 2, and 0.78 for IGG ≥ 3 vs. IGG ≤ 2. The corresponding figures for biparametric MRI (RADC and RT2w) were 0.63 and 0.59. mpMRI (RKtrans, RADC and RT2w) increased the AUCs to 0.74 for IGG 3 vs. IGG 2 and 0.75 for IGG ≥ 3 vs. IGG ≤ 2 (p < 0.01). Combining PSMA-SUVmax with mpMRI further increased the AUCs to 0.82 (p < 0.05) and 0.84 (p < 0.01), respectively. See Fig. 1 for a selection of ROC curves.
Conclusion
The clinically important distinction between ISUP grade groups 2 and 3 could be reflected in partially discriminative cut-off values derived from PSMA-PET, Acetate-PET and mpMRI. The results also indicate that the imaging methods provide independent information. However, ADC-maps and T2w images contributed less to the differentiation between ISUP grade groups.