Effect of early fractional lymphocyte loss on lymphopenia probability models for NSCLC
PO-2122
Abstract
Effect of early fractional lymphocyte loss on lymphopenia probability models for NSCLC
Authors: Takahiro Kanehira1, Hiroshi Taguchi2, Norio Katoh3, Yusuke Uchinami4, Takaaki Yoshimura5, Masaya Tamura1, Ryusuke Suzuki1, Takayuki Hashimoto6, Hidefumi Aoyama4
1Hokkaido University Hospital, Department of Medical Physics, Sapporo, Japan; 2Hokkaido University Hospital, Department of Radiation Oncology, Sapporo, Japan; 3Hokkaido University, Department of Radiation Oncology, Faculty of Medicine and Graduate School of Medicine, Sapporo, Japan; 4Hokkaido University, Department of Radiation Oncology, Faculty of Medicine and Graduate School of Medicine, Sapporo, Japan; 5Hokkaido University, Department of Health Sciences and Technology, Faculty of Health Sciences, Sapporo, Japan; 6Hokkaido University, Department of Radiation Medical Science and Engineering, Faculty of Medicine, Sapporo, Japan
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiotherapy (RT) for NSCLC causes radiation-induced lymphopenia (RIL) possibly affecting survival. In a recent study, fractional lymphocyte loss (FLL) observed in early radiation fractions was related to overall reduction in absolute lymphocyte count (ALC) for several tumor sites, which can be used to predict RIL. For a lung region, however, FLL and its effect on RIL prediction are unknown. This study aimed to evaluate whether FLL improves RIL probability model for NSCLC patients.
Material and Methods
We included 84 stage Ⅰ-Ⅲ NSCLC patients who received concurrent chemo-radiotherapy between 2011 and 2022 in our hospital. Prescribed dose of 60 Gy in 30 fractions (Fx) or 66 Gy in 33 Fx to planning target volume was delivered with either/both 3D-CRT or/and IMRT. ALCs were collected from blood tests from 1 week before RT start till 1 week after RT completion, and nadir ALC was defined after RT start. To estimate FLL, as Ellsworth et al. (2020), we fitted an exponential curve to ALCs plotted against radiation fractions prior to 16th Fx for each patient:  (x: fraction number, a and b: fitting parameters). FLL was calculated as
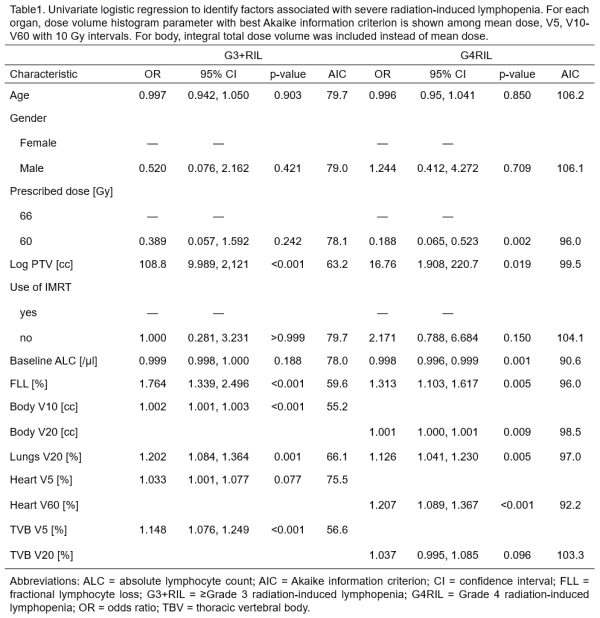
(x: fraction number, a and b: fitting parameters). FLL was calculated as  . As endpoints, nadir ALC was evaluated for ≥Grade 3 and Grade 4 lymphopenia (G3+RIL and G4RIL) (CTCAE v.5.0). Univariate logistic regression analyses (UVA) associated dose volume histogram (DVH) and non-DVH parameters with endpoints. Factors with p-value <0.2 and best Akaike information criterion (AIC) among DVH parameters for each organ at risk in UVA were included in multivariate logistic regression analyses (MVA), and forward stepwise variable selections were used based on p-value <0.05. To access effects of FLL on models, we also performed MVA without FLL. Receiver operating characteristic analyses were performed to evaluate model discriminations using area under the curve (AUC).
. As endpoints, nadir ALC was evaluated for ≥Grade 3 and Grade 4 lymphopenia (G3+RIL and G4RIL) (CTCAE v.5.0). Univariate logistic regression analyses (UVA) associated dose volume histogram (DVH) and non-DVH parameters with endpoints. Factors with p-value <0.2 and best Akaike information criterion (AIC) among DVH parameters for each organ at risk in UVA were included in multivariate logistic regression analyses (MVA), and forward stepwise variable selections were used based on p-value <0.05. To access effects of FLL on models, we also performed MVA without FLL. Receiver operating characteristic analyses were performed to evaluate model discriminations using area under the curve (AUC).
Results
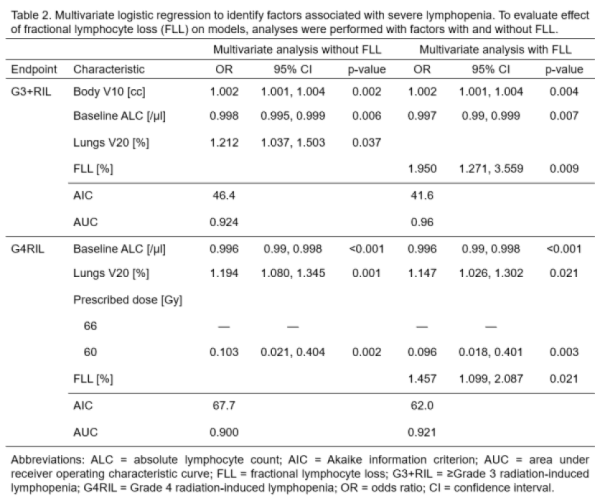
Baseline ALC was 1614 [/μl] (IQR:1352 to 2066) and incidence rates were 83% (n=70) for G3+RIL and 30% (n=25) for G4RIL. By exponential curve fitting to the early lymphocyte changes, FLL was found to be a median of 7.1% (IQR: 5.1% to 8.9%). With factors selected from UVA (Table 1), MVA revealed that FLL was significantly associated with both G3+ and G4RIL (Table 2), resulting in better model quality (lower AIC) with slightly higher AUC compared to models without FLL: AUC of 0.96 and 0.92 with and without FLL for G3+RIL and 0.92 and 0.90 for G4RIL respectively. In addition to FLL, lower baseline ALC as well as higher body V10 [cc] and lungs V20 [%] was associated with increasing G3+ and G4RIL risks respectively. For G4RIL, prescribed dose difference remained significantly associated.
Conclusion
Incorporating FLL into severe lymphopenia probability models improved model quality with modest changes in discrimination capability. A larger cohort is needed to conclude these findings.