A method to explore dose and LET for normal tissue response studies in large proton therapy cohorts
Rasmus Klitgaard,
Denmark
PO-2091
Abstract
A method to explore dose and LET for normal tissue response studies in large proton therapy cohorts
Authors: Rasmus Klitgaard1,2, Perry Johnson3, Nancy P. Mendenhall3, Mark Artz3, Curtis Bryant3, Peter Lægdsmand1,2, Lars Fredrik Fjæra4, Ludvig P. Muren1,2
1Aarhus University, Department of Clinical Medicine, Aarhus, Denmark; 2Aarhus University Hospital, Danish Centre for Particle Therapy, Aarhus, Denmark; 3University of Florida College of Medicine, Department of Radiation Oncology, Jacksonville, FL, USA; 4University of Bergen, Department of Physics and Technology, Bergen, Norway
Show Affiliations
Hide Affiliations
Purpose or Objective
Normal tissue complication probability (NTCP) calculations in proton therapy (PT) are usually
performed using models derived from photon-based radiotherapy, with the assumption of a constant
relative biological effectiveness (RBE) of 1.1. However, RBE has been shown to vary with dose
weighted linear energy transfer (LETd), which is often not considered by NTCP models. LETd
distributions can be obtained by use of Monte Carlo simulations (MC). However, there is currently no
consensus on how to analyze LETd in larger cohorts, nor on how to include LETd in proton-specific
NTCP models.
In this work we seek to explore a method of analyzing dose and LETd distributions with respect to
morbidity, based on multiple pairs of dose and LETd thresholds, in a large cohort of prostate cancer
patients treated with passively scattered PT.
Material and Methods
For the organ of interest we iteratively selected a dose threshold and from the sub-region of the organ with a
dose higher than this threshold, we selected an LETd threshold. For each combination we then graphed the
dose threshold vs. the LETd threshold for each patient, with color-coding for patients with vs. without
morbidity.
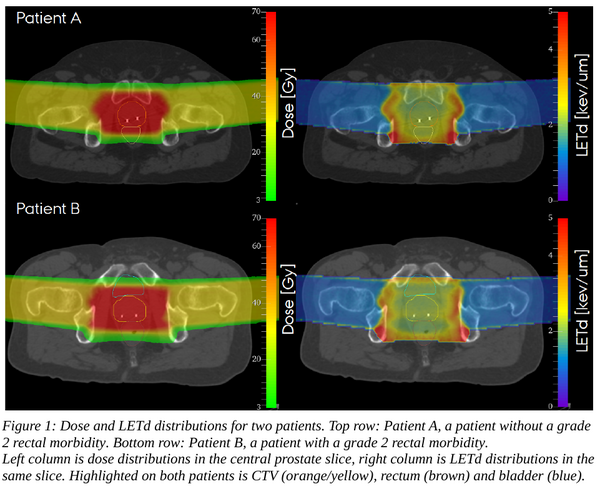
The method was explored on grade 2 rectal morbidity data from a sub-cohort (n=111) of a large passively
scattered PT prostate cancer cohort (n=1214), treated to 78 Gy(RBE 1.1) and morbitities recorded
prospectively up to 8 years (incidence ~15% for both full and sub-cohort). MC simulations in FLUKA with a
validated implementation of the gantry were conducted with 200 million primaries per treatment field,
scoring LETd and dose (figure 1).
Results
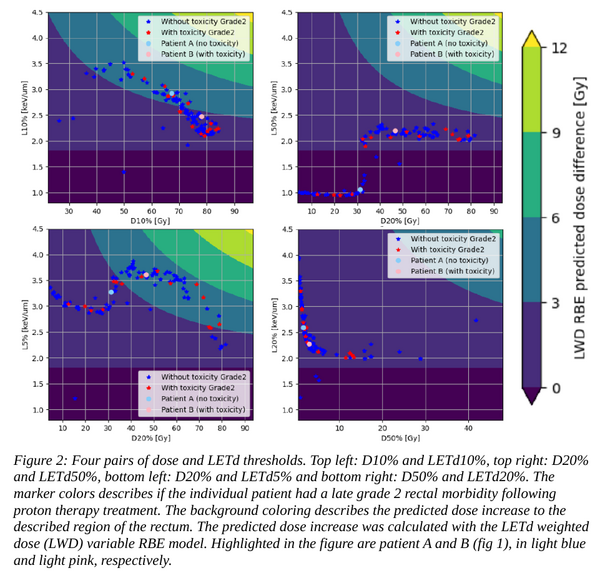
Figure 2 shows the resulting distributions using four different pairs of dose and LETd thresholds. The
distributions visualize the extent of variation in different areas of the dose and LETd volume space, and thus
where potential differences between patients with vs. without morbidity can be observed.
E.g. for the D10% and LETd10% thresholds, the D10% of the rectum for our cohort varied from 30 Gy to
above 80 Gy, with the majority above 60 Gy. The LETd10% for the high dose region of the rectum ranged
from 1.5 keV/um to above 3.5 keV/um. However, there were no observed differences between with patients
with vs. patient without grade 2 rectal morbidity.
Conclusion
We have developed a method to explore the potential impact of LETd for a selected LETd threshold within a
dose threshold, applied on rectal morbidity data for prostate cancer patients. In the present analysis of our
sub-cohort, we did not see any separation in the data for patients with vs. without rectal morbidity.