Deep learning-based classification of Xerostomia in ARTSCAN III patients
PO-2083
Abstract
Deep learning-based classification of Xerostomia in ARTSCAN III patients
Authors: Viktor Rogowski1, Mustafa Kadhim1, Christian Jamtheim Gustafsson2, Maria Gebre-Medhin2, Per Munck af Rosenschöld1, Andre Änghede Haraldsson1
1Hematology, Oncology and Radiation Physics, Skåne University Hospital, Lund, Sweden, Hematology, Oncology and Radiation Physics, Skåne University Hospital, Lund, Sweden, Lund, Sweden; 2Department of Hematology Oncology and Radiation Physics, Skåne University Hospital, Lund, Sweden, Department of Hematology Oncology and Radiation Physics, Skåne University Hospital, Lund, Sweden, Lund, Sweden
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiation-induced xerostomia (mouth dryness) is a common side-effect post treatment of Head and Neck cancer. Previous prospective clinical data is scarce. Some data suggest that radiation dose to some parts of the salivary glands correlates better with xerostomia than the commonly used average dose to the entire glands. In this work, we aim to construct models based on dosimetry on treated patients. In addition, we attempt to use Deep Learning (DL) methods to correlate spatial dose and image data with xerostomia outcomes and further discriminate which dose and anatomies should be spared in radiotherapy.
Material and Methods
Late xerostomia outcomes data from 298 patients included in the prospective clinical trial (ARTSCAN III) was collected. Xerostomia outcomes were classified as an event if grade 2+ and a no occurring xerostomia class (grade 0-1). First, a forward conditional logistic regression model was fitted to the xerostomia outcomes based on smoking status, age, BMI, T-stage, average dose to the oral cavity, submandibularis glands, and to the bilateral parotid glands. Secondly, for a subset of the patients (158) where 3D image and dosimetry data were available. A balanced sub data set was used as training data. The data was inserted into a 3D ResNet-18 model consisted of CT-scans, 3D dose distributions, organs at risk binary masks (parotid gland, submandibular glands, oral cavity) and toxicity indication. Offline data augmentation was used during training and the data was randomly split as 75% training, 20% validation and 5% test. The test data was hidden from the model during training.
Results
Data from 245 patient was included in the logistic regression model. The dose metrics were internally correlated with Spearman rho’s ranging from 0.1-0.5 (p<0.05). Logistic regression revealed that only the average bilateral dose to the parotid glands were significantly contributing to xerostomia prediction (p<0.001). The model parameters were: D50=19.33 Gy and gamma50=0.23 (see Fig 2), confidence intervals were derived using Boot-strapping (10000 samples). The DL model accuracy was 70% on the validation data set and 40% on the test data set. These preliminary results reveal that the DL model currently was unable improve upon conventional statistical regression model analysis, and that (currently) spatial correlations and image data did not reveal additional information to the augment the model in predicting xerostomia grade 2. 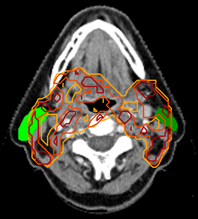 Figure 1. Outlined parotid glands with dose distribution.
Figure 1. Outlined parotid glands with dose distribution.
Conclusion
A logistic regression model revealed that D50 equaled 19 Gy for the average bilateral parotids in this data set. The DL model indicated the need to expand the dataset and conduct extensive cross-validation model tuning. Additional data sets may be needed to improve the accuracy of the DL model compared to traditional regression analysis.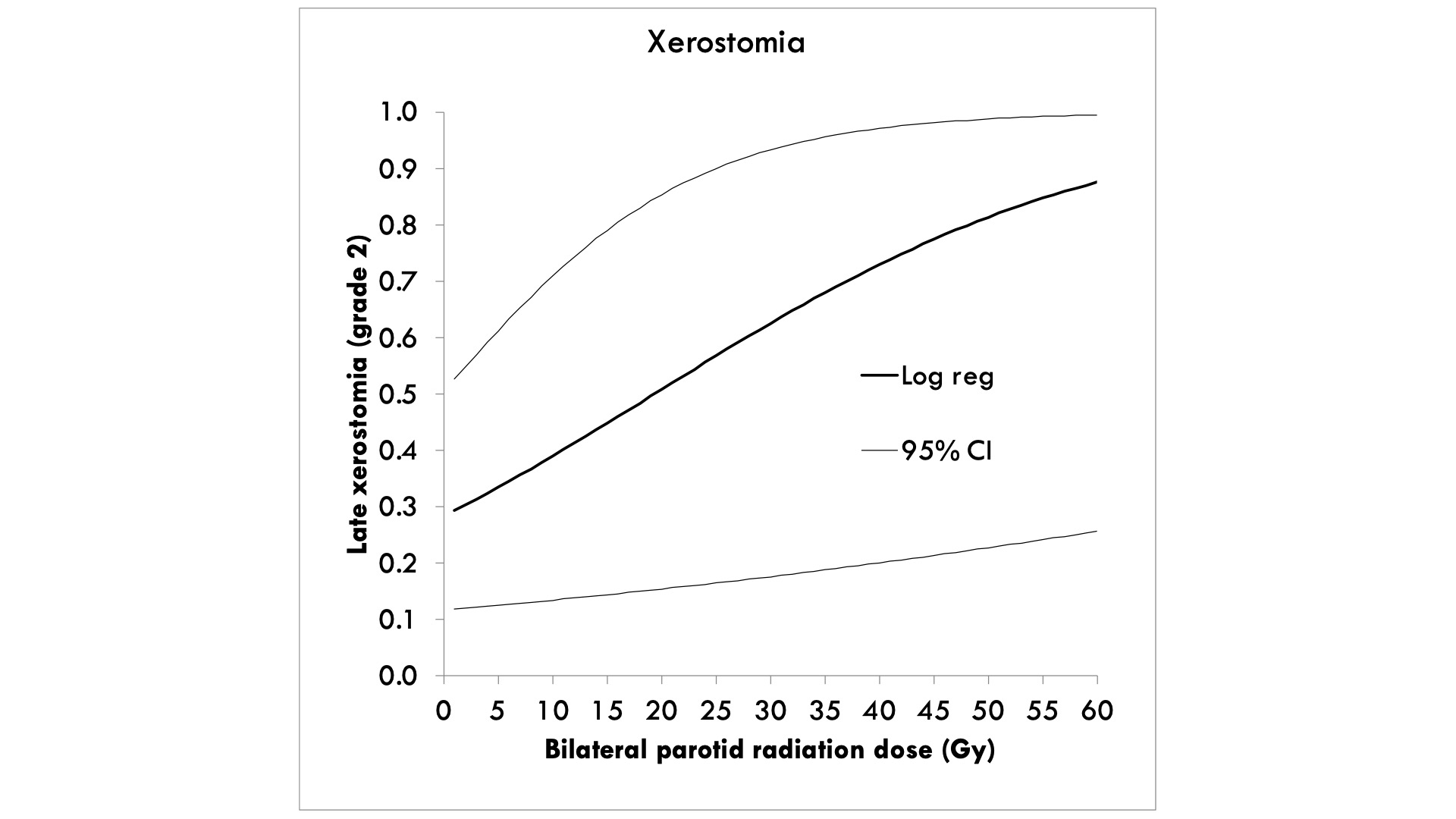 Figure 2. The model parameters were: D50=19.33 Gy and gamma50=0.23.
Figure 2. The model parameters were: D50=19.33 Gy and gamma50=0.23.