SYNERGISTIC EFFECT OF STEREOTACTIC RADIOTHERAPY AND IMMUNOTHERAPY: AN ITALIAN MULTICENTRIC STUDY
PO-1608
Abstract
SYNERGISTIC EFFECT OF STEREOTACTIC RADIOTHERAPY AND IMMUNOTHERAPY: AN ITALIAN MULTICENTRIC STUDY
Authors: Anna Gorza1,3, Giuseppe Fanetti2, Vittorio Baggio1, Irene Turturici2, Oscar Servodio4, Alberto Revelant2, Francesca Gessoni2,3, Antonio Fabio Stefano Minissale1, Fabio Matrone2, Federica Bertini2, Alessandra Donofrio2, Mario Moro5, Paola Chiovati6, Fabio Ferrarese1, Maurizio Mascarin2
1AULSS 2 Marca Trevigiana, Treviso Hospital, Division of Radiation Oncology, Treviso, Italy; 2Centro di Riferimento Oncologico di Aviano (CRO) IRCCS, Division of Radiation Oncology, Aviano, Italy; 3University of Padua, Department of Medicine DIMED, Padua, Italy; 4AULSS 2 Marca Trevigiana, Treviso Hospital, Division of Radiation Oncology, Aviano, Italy; 5AULSS 2 Marca Trevigiana, Treviso Hospital, Division of Neurosurgery, Treviso, Italy; 6Centro di Riferimento Oncologico di Aviano (CRO) IRCCS, Division of Medical Physics, Aviano, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
To evaluate the oncologic outcome, toxicity and prognostic factors associated with outcome of the combined treatment with Immune Checkpoint Inhibitors (ICIs) and Stereotactic Radiotherapy (SRT) in patients with metastatic disease from different primary malignancies.
Material and Methods
A retrospective multicenter cohort of metastatic patients treated with ICIs and SRT for oligometastatic (OMD) or oligoprogressive disease (OPD) was performed. Descriptive statistics was used to evaluate patient and treatment related features. Progression-Free Survival (PFS), Overall Survival (OS) and Therapy switch-Free Survival (TS-FS) were analyzed using Kaplan-Meyer curves and log rank testing. The cumulative incidence of local recurrence (LR) was estimated through the Kaplan-Meier method according to the Fine-Gray model. Toxicity was evaluated through CTCAE v 5.0 scale.
Results
Between 2014 and 2022, 27 patients were treated with SRT to 53 lesions for OMD or OPD during ICIs. OPD was found in 23 (85%) patients. 19 (70%) patients were male and 15 (56%) patients were older than 65 years. Initial diagnosis was melanoma, lung cancer, renal cancer and head and neck cancer in 10 (37%), 12 (44%), 4 (15%) and 1 (4%) patients respectively. Median SRT total dose was 27 Gy (range 24-30 Gy) delivered in 3 fractions (range 3-5) and irradiated metastatic lesions were in brain, lymph nodes, lung and others in 32 (60%), 9 (17%), 7(13%) and 5(9%), respectively. After SRT, patients were followed for a median follow up of 11.3 months. One-year PFS, TS-FS and OS were 39.5%, 45% and 73%, respectively (Figure 1).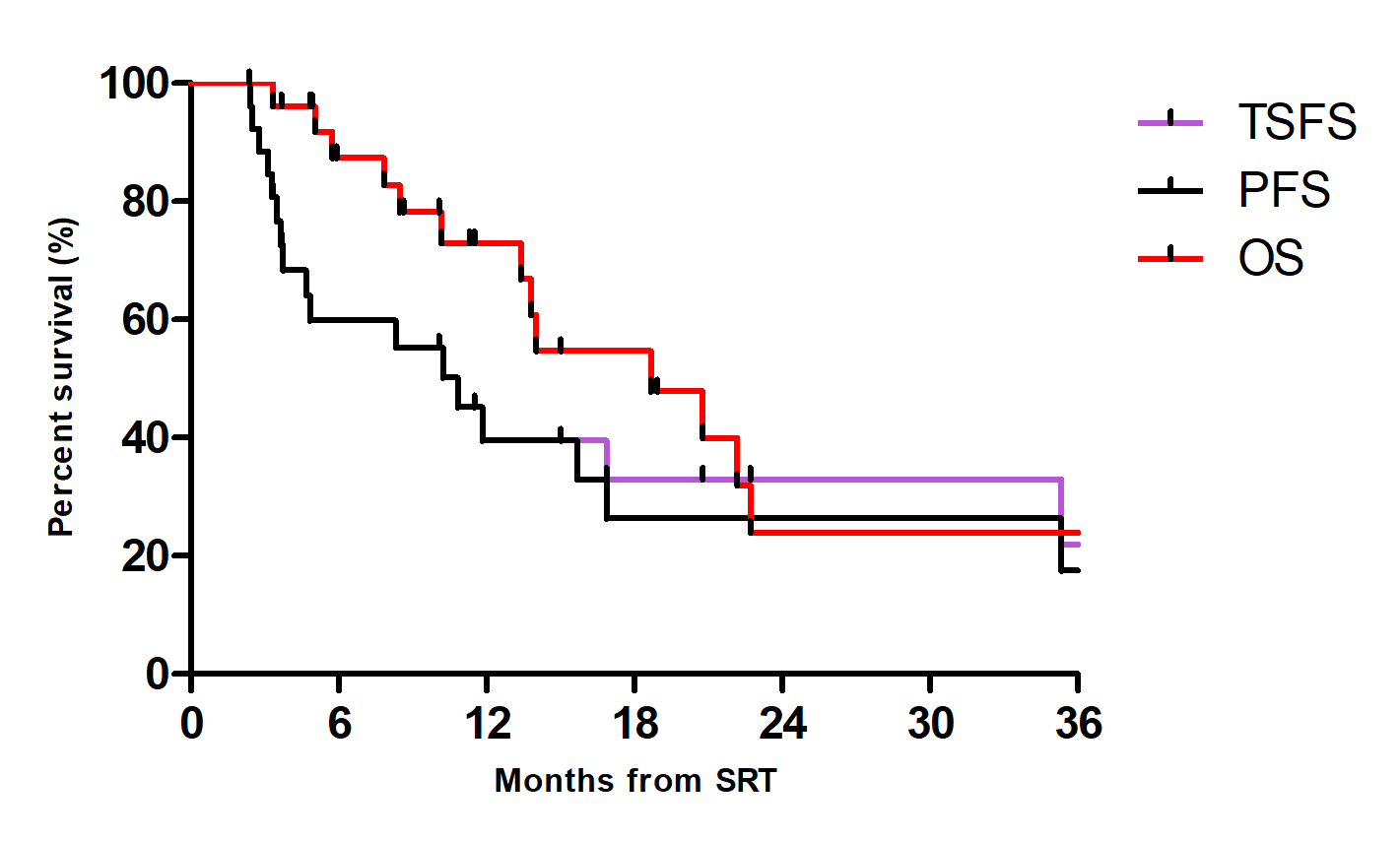 Median PFS was 8.2 months and median OS was 18.3 months. Median TS-FS was 10.2 months, with an average Time to Treatment Switch (TTS) of 11 months for all patients who changed systemic therapy and an average TTS of 31.5 months for patients who underwent SRT two or more times for oligoprogressive disease. Concomitant chemotherapy, higher Charlson Comorbidity Index, brain as first site of SRT and low lymphocyte count were predictive factors of LR. Only four patients experienced treatment related toxicity (grade 1 to 3).
Median PFS was 8.2 months and median OS was 18.3 months. Median TS-FS was 10.2 months, with an average Time to Treatment Switch (TTS) of 11 months for all patients who changed systemic therapy and an average TTS of 31.5 months for patients who underwent SRT two or more times for oligoprogressive disease. Concomitant chemotherapy, higher Charlson Comorbidity Index, brain as first site of SRT and low lymphocyte count were predictive factors of LR. Only four patients experienced treatment related toxicity (grade 1 to 3).
Conclusion
The combination stereotactic radiotherapy and immunotherapy is safe and allows to postpone the initiation of a new line of systemic therapy of about 11 months with a very favorable toxicity profile. Results in terms of survival are encouraging. Further research is needed to evaluate the optimal integration between immunotherapy and local therapies and SRT in particular as well as to identify predictive biomarkers. We aim at understanding the role of systemic inflammation biomarkers in this scenario.