Stereotactic Arrhythmia Radioablation for Ventricular Tachycardia: Single Center Experience
PO-1597
Abstract
Stereotactic Arrhythmia Radioablation for Ventricular Tachycardia: Single Center Experience
Authors: Federico Colombo1, Francesco Salaroli2, Ilaria Renna2, Elisabetta Lattanzi2, Giovanni Ceccon2, Stella Gianni2, Claudia Grondelli2, Marialuisa Bergamini2, Cristina Dell'Anna2, Marco Galaverni2, Giovanna Benecchi3, Gianluca Gonzi4, Maria Francesca Notarangelo4, Alessandro Palumbo5, Caterina Ghetti3, Nunziata D'Abbiero2, Nicola Simoni2
1Azienda Ospedaliero Universitaria di Parma - Scuola di Specializzazione UNIMORE, Radiation Oncology Unit, Parma, Italy; 2Azienda Ospedaliero Universitaria di Parma, Radiation Oncology Unit, Parma, Italy; 3Azienda Ospedaliero Universitaria di Parma, Medical Physics Unit, Parma, Italy; 4Azienda Ospedaliero Universitaria di Parma, Cardiology Unit, Parma, Italy; 5Azienda Ospedaliero Universitaria di Parma, Radiology Unit, Parma, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Stereotactic Ventricular Arrhythmia Radioablation (STAR) has emerged as a promising treatment option to precisely ablate the arrhythmogenic substrate of scar-related refractory ventricular tachycardia (rVT), in patients at prohibitive risk for catheter ablation (CA).
Material and Methods
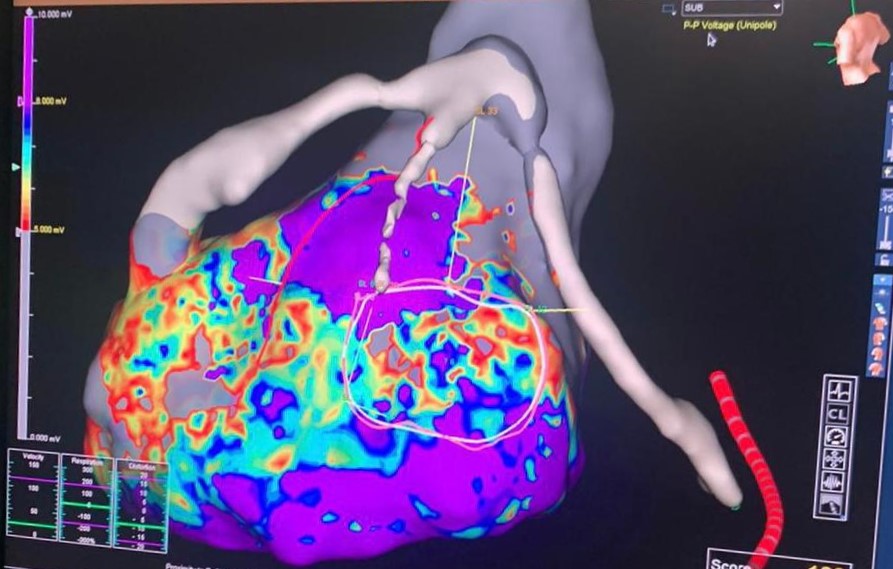
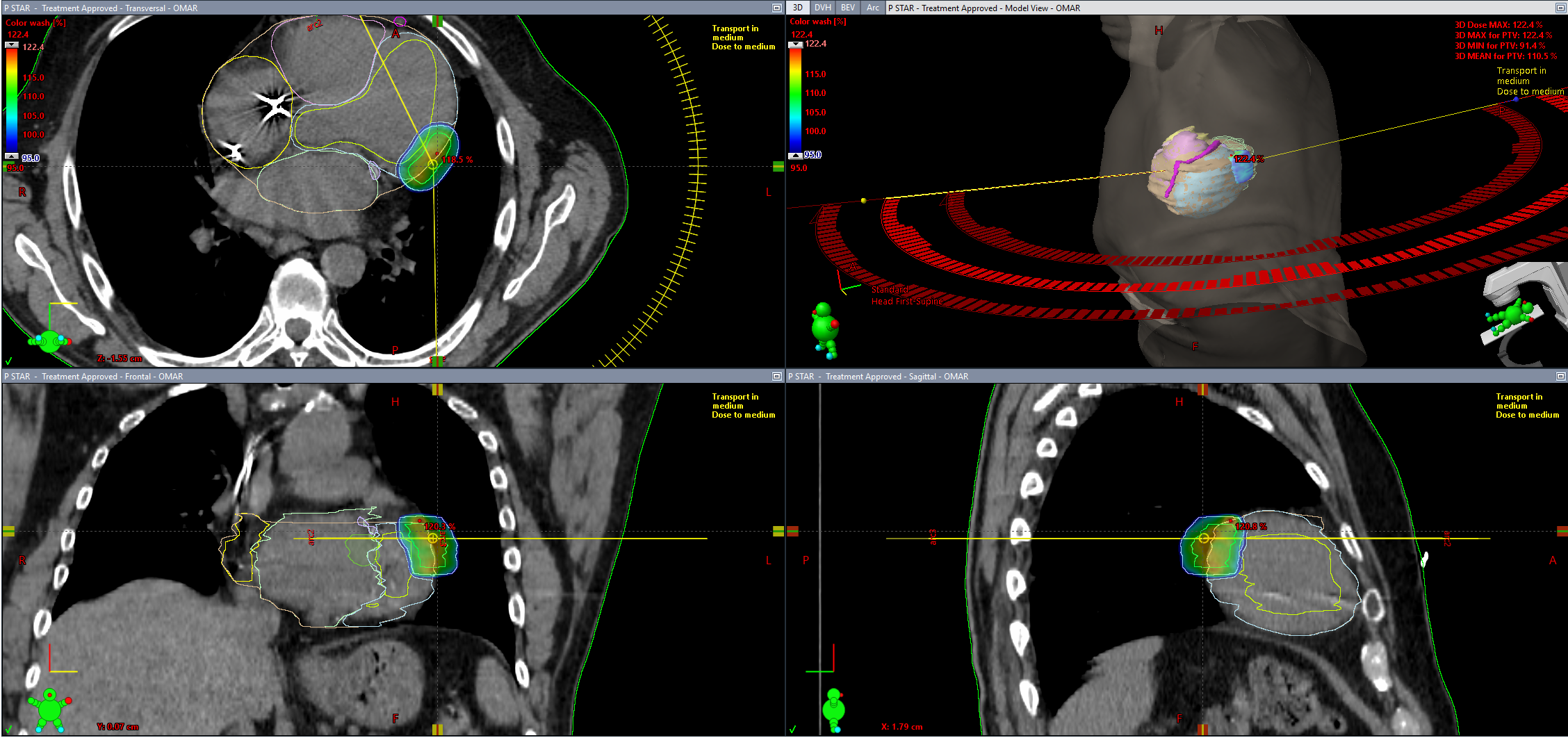
We present the experience with the first 2 patients treated with STAR for rVT at our Institution. The first patient treated was an 87-years-old man, hospitalised for rVT requiring ICD interventions, unresponsive to antiarrhythmic drugs. The second patient was a 60-years-old man, with rVT secondary to ischemic cardiomyopathy, presenting to the emergency department in VT storm requiring multiple ICD shocks and not responsive to maximal antiarrhythmic therapy. Both patients were considered not eligible for CA due to high intraprocedural risks. For target localization, high-density substrate electroanatomic cardiac mapping, cardiac computed tomography (CT) and magnetic resonance (MR) were acquired. To manage cardiac motion, a four-dimensional (4D) CT-simulation was adopted. Target volume definition was defined by Radiation Oncologists in cooperation with Electrophysiologists and dedicated Radiologists.
Results
STAR was delivered using 3 co-planar arcs configuration Volumetric Modulated Arc Therapy (VMAT). A photon energy of 6MV, flattening filter free (FFF) technique, and a dose rate of 1400 MU/min were used for both treatments. The prescribed dose was 25 Gy in single fraction to the Planning Target Volume, with a Dmax of 32 Gy to the arrhythmogenic substrate. To optimize image-guidance, a Cone Beam CT (CBCT) was performed before each arc delivery, and a respiratory-gated approach was used to monitor patients during fraction. The first patient was discharged from the hospital 1 week after STAR, while the second patient after 3 weeks. No acute or late toxicities related to STAR were reported. At 8 months and 4 months follow up for the first and second patients, respectively, no rVT were recorded during in hospital clinical evaluation and home monitoring ICD interrogation.
Conclusion
The present report confirms the efficacy and safety of STAR as a reasonable treatment option for patients with rVT not suitable for CA. Further investigations and longer follow up are needed to draw definitive conclusions.