Palliative care assessment in glioblastoma multiforme treated in a radiotherapy department.
Mercedes Gonzalez Cantero,
Spain
PO-1588
Abstract
Palliative care assessment in glioblastoma multiforme treated in a radiotherapy department.
Authors: Beatriz Deben Mendez1, Marta Rodriguez Roldan2, Maria Isabel Garrido Botella1, Elisabeth Gonzalez Del Portillo1, Abrahams Alexis Ocanto Martinez3, Mercedes Gonzalez Cantero1, Macarena Teja Ubach1, Rafael Rosel Aller1, Daniel Martinez Perez4, Jorge Pedregosa Barbas4, Jose Angel Garcia Cuesta4, Celia García Torres5, Ana Castaño Cantos1, Yolanda Vilches Aguirre6, Alberto Alonso Babaro6, Rosa Maria Morera Lopez2
1Hospital Universitario La Paz, Radiation oncology department, Madrid, Spain; 2Hospital universitario La Paz, Radiation oncology department, Madrid, Spain; 3Hospital Universitario de Torrejón, Radiation oncology department, Madrid, Spain; 4Hospital Universitario La Paz, Medical oncology department, Madrid, Spain; 5Hospital Universitario Rey Juan Carlos, Radiation oncology department, Madrid, Spain; 6Hospital Universitario La Paz, Palliative care department, Madrid, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
Glioblastoma multiforme (GBM) is an infiltrating astrocytic tumor with a poor prognosis and a median survival of 12 months. Its standard treatment consists of
maximal resection followed by STUPP (concomitant radiotherapy (RT) and temozolamide (TMZ) and 6 cycles of subsequent TMZ). The aim of this study was to report the proportion of patients who completed the full treatment regimen, and the proportion who were referred to palliative care (PC).
Material and Methods
Retrospective descriptive study. Sample of 144 patients evaluated in a radiotherapy oncology service in a tertiary hospital diagnosed with high-grade glioma treated with RT from January 2016 to December 2019. We analysed clinical variables and possible prognostic factors for survival: whether patients completed the STUPP scheme, whether they completed RT treatment, whether they were assessed for PC and the median time between PC assessment and exitus.
Results
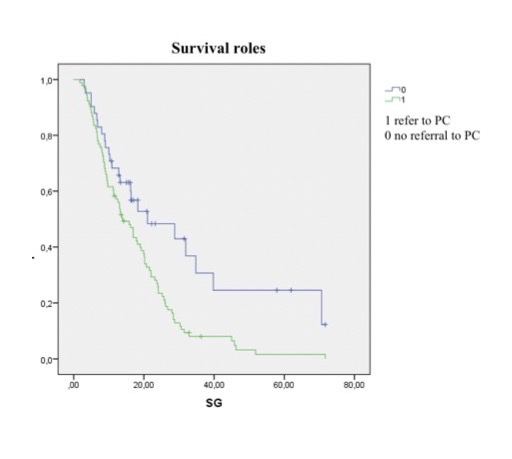
Among the 144 patients, 31 (21.5%) completed this standard treatment. RT treatment was completed by 92.4%. 66.7% of patients were assessed by a PC unit, with a median survival time between assessment and exitus of 1.68 months. Referral to PC was statistically significant as a prognostic factor for poorer survival (p<0.004).
Conclusion
This study indicates that patients with GBM complete a high percentage of RT treatment. However, few are referred to PC, with this referral being a prognostic factor for poorer survival, probably due to the funcional deterioration that occurs when this is done late. It is worth investigating whether earlier referral to PC would lead to a better prognosis.