Immunomodulation by partial tumor irradiation using and carbon-ions: bystander and abscopal effects
PO-1586
Abstract
Immunomodulation by partial tumor irradiation using and carbon-ions: bystander and abscopal effects
Authors: Slavisa Tubin1, Piero Fossati2, Giovanna Martino3, Joanna Gora2, Antonio Carlino3, Eugen Hug2
1Medaustron Center for Ion Therapy, Radiation Oncology, Wiener Neustadt, Austria; 2Medaustron, Radiation Oncology, Wiener Neustadt, Austria; 3Medaustron, Medical Physics, Wiener Neustadt, Austria
Show Affiliations
Hide Affiliations
Purpose or Objective
A novel approach for PArtial Tumor irradiation of HYpoxic segment (PATHY) sparing the Peritumoral Immune Microenvironment (PIM) was developed with the purpose to improve the radiotherapy-therapeutic ratio of unresectable bulky tumors. This immunomodulatory approach was designed to add to direct radiation tumor cell killing also the component of immune-mediated killing measured as bystander and abscopal effect. The hypothesis is that for effective immunomodulation, the entire tumor volume may not need to be irradiated but only a partial volume to initiate the immune cycle in radiation-spared PIM. The aim was to assess the impact of PATHY on QoL, tumor downsizing, tumor control and survival among patients affected by recurrent unresectable bulky tumors unsuitable for conventional radiotherapy. Impact of this approach on tumor control and survival among patients who failed previous state-of-the-art treatments was reported.
Material and Methods
11 consecutive patients were treated between March 20 and December 21 (Fig.1).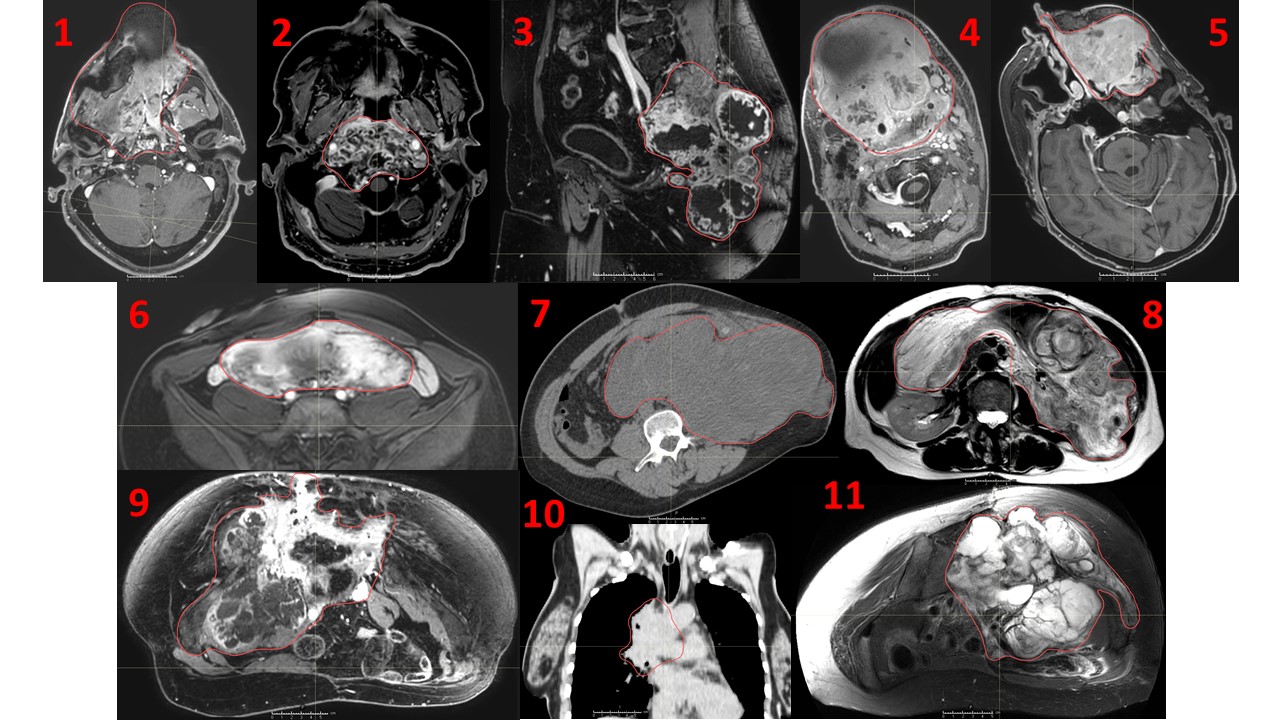 According to the Palliative Prognostic Index, all patients had a life expectancy of <3months. 63% of patients had sarcoma while 37% head and neck or lung unresectable bulky cancers. The hypoxic tumor segment, corresponding on average to approximately 30% of the GTV volume, was irradiated with 30, 36 or 45 Gy RBE in 3 fractions. PIM was created as a uniform 1 cm large ring surrounding the GTV and was protected by highly conservative constraints: Dmean<5Gy, D20%<0.2Gy, D50%<1Gy. 45% of patients previously received at least 1 course of radiotherapy (18% already re-irradiated). In addition to bulky disease, 45% of patients had metastatic lesions. All patients were symptomatic.
According to the Palliative Prognostic Index, all patients had a life expectancy of <3months. 63% of patients had sarcoma while 37% head and neck or lung unresectable bulky cancers. The hypoxic tumor segment, corresponding on average to approximately 30% of the GTV volume, was irradiated with 30, 36 or 45 Gy RBE in 3 fractions. PIM was created as a uniform 1 cm large ring surrounding the GTV and was protected by highly conservative constraints: Dmean<5Gy, D20%<0.2Gy, D50%<1Gy. 45% of patients previously received at least 1 course of radiotherapy (18% already re-irradiated). In addition to bulky disease, 45% of patients had metastatic lesions. All patients were symptomatic.
Results
Median follow up was 7.2 months (range 3–22). Average GTV tumor volume was 1460cc (range 76-5646). Average treated tumor volume was 431cc corresponding to 29.6% of the GTV tumor volume. PIM was effectively spared. Overall survival and progression-free survival at last follow up were 64% and 46%, respectively. Median patient survival was 7.1 month (estimated was < 3 months). Local tumor control at last follow up was 46% following the single PATHY course. Bystander effect, mesured as a significant GTV volume reduction, was induced in 73% of patients. Average GTV volume reduction was 60%. In 3 out of 5 metastatic patients (60%) abscopal effects were reported (Fig. 2).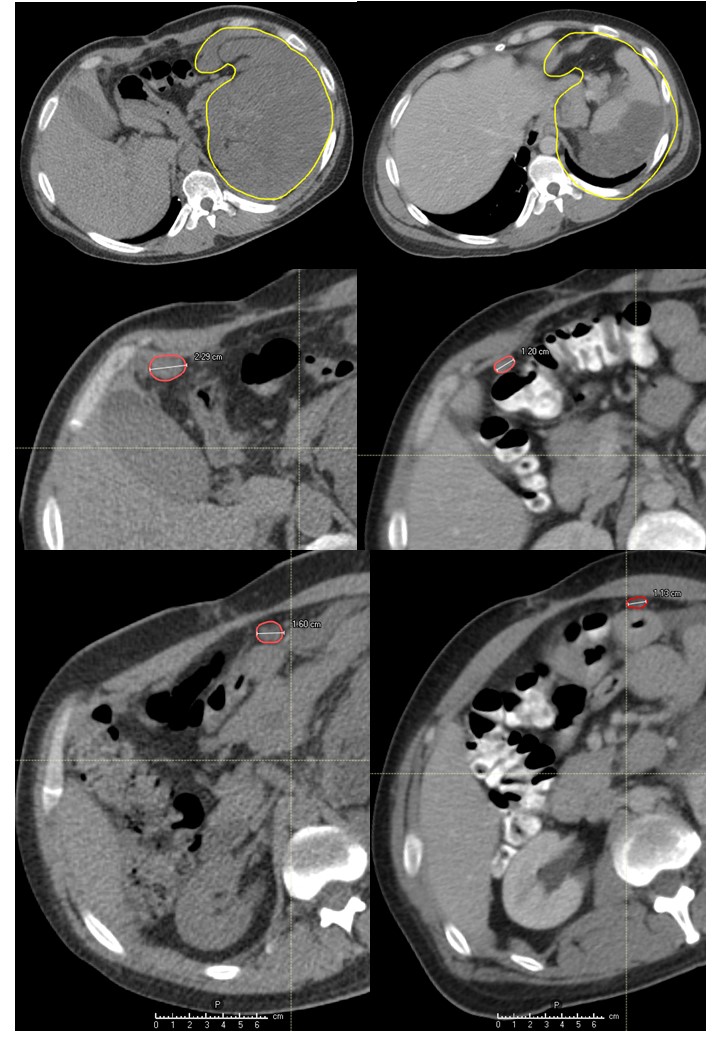
Symptom relief was achieved in all but 1 patient (91%). 27% of patients presented G1-2 fatigue and no other side effects.
Conclusion
The PATHY-radiotherapy was effective, safe and well tolerated treatment. It resulted in improvement in symptoms and quality of life of highly complex patients without associated treatment related toxicity. This approach showed high immunogenic potential resulting in varying degrees of tumor downsizing/neoadjuvant effect with average tumor shrinkage corresponding to 60%. Optimum patient selection and definition of most suitable disease characteristics are currently explored in an ongoing, prospective study.