Pediatric anesthesia for external beam proton therapy. Local experience
Mikhail Cherkashin,
Russian Federation
PO-1568
Abstract
Pediatric anesthesia for external beam proton therapy. Local experience
Authors: Mikhail Cherkashin1, Alexey Nikolaev2, Nikolay Vorobyov3, Fatima Valieva2, Albina Gokoeva2, Nikita Berezin4, Konstantin Boiko5, Natalya Martynova3, Kirill Suprun6, Natalia Berezina7
1Medical Institute n.a.Berezin Sergey, Oncology, St Petersburg, Russian Federation; 2Medical Institute n.a.Berezin Sergey, Anesthesia, St Petersburg, Russian Federation; 3Medical Institute n.a.Berezin Sergey, Proton Therapy, St Petersburg, Russian Federation; 4Medical Institute n.a.Berezin Sergey, Simulation center, St Petersburg, Russian Federation; 5Medical Institute n.a.Berezin Sergey, Pediatric Oncology, St Petersburg, Russian Federation; 6Medical Institute n.a.Berezin Sergey, Medical Quality Management, St Petersburg, Russian Federation; 7Medical Institute n.a.Berezin Sergey, Administrative, St Petersburg, Russian Federation
Show Affiliations
Hide Affiliations
Purpose or Objective
To discuss anesthesia management for proton beam therapy in pediatric oncology.
Material and Methods
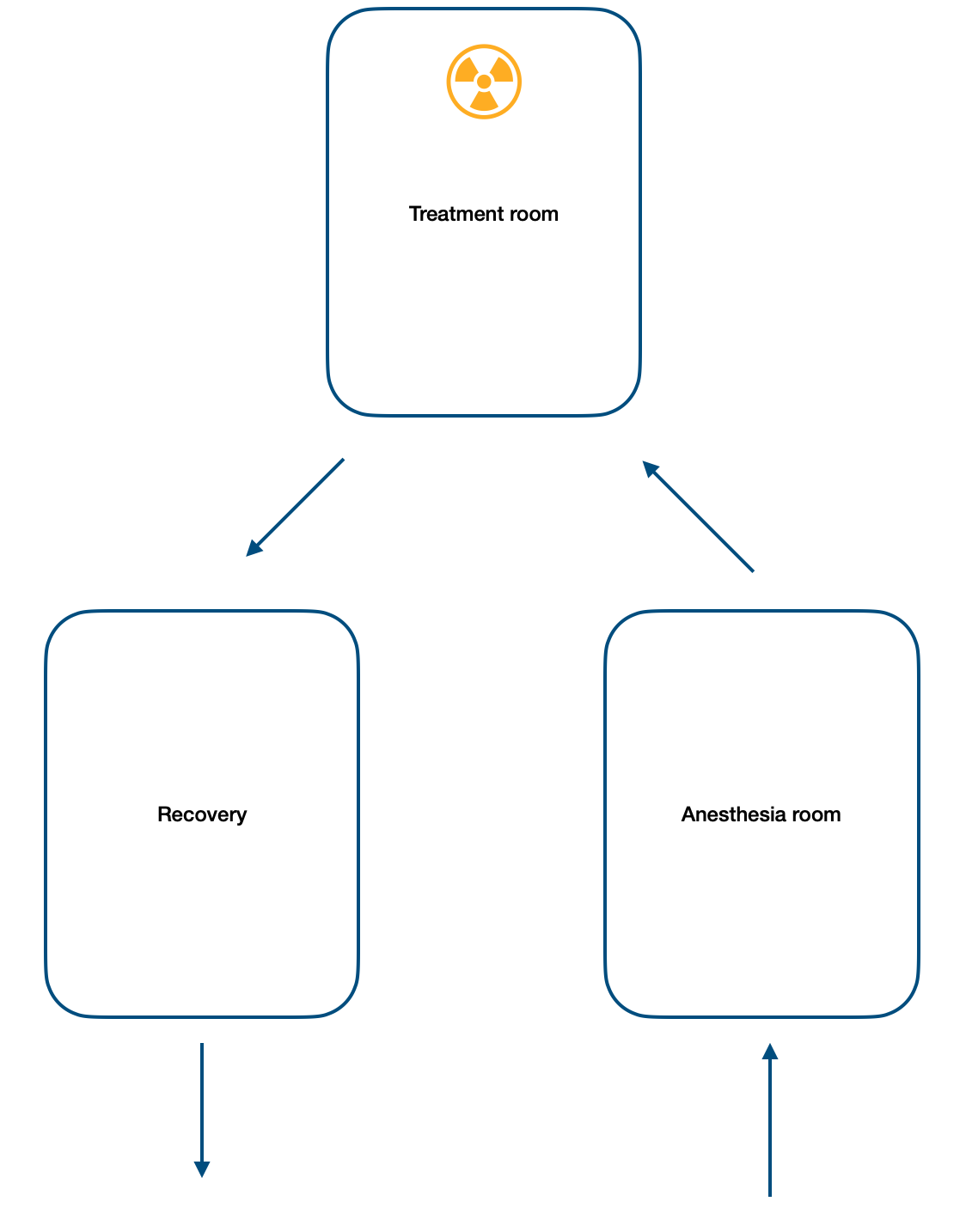
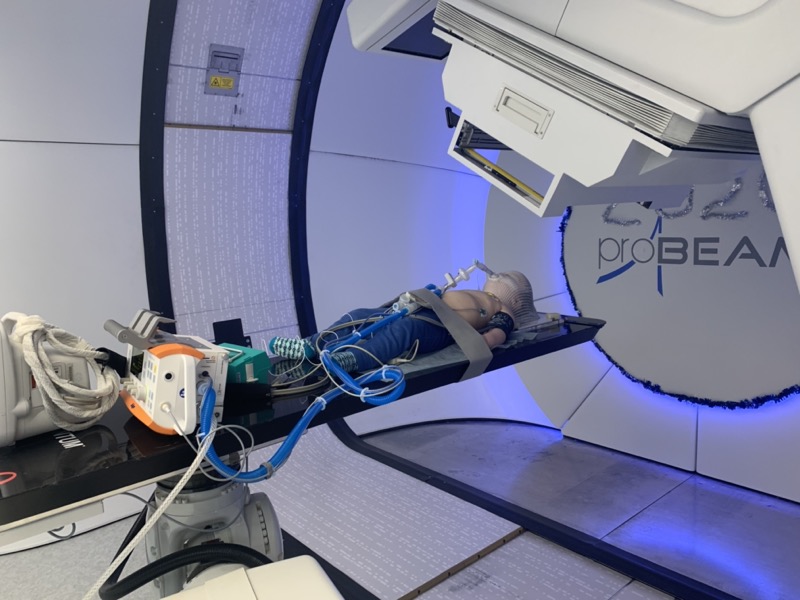
During 2018 - 2021 in our hospital 876 children with CNS and body tumors received proton therapy. In 360 cases radiation treatment delivered with anesthesia. Mean fractions number was 34 (anesthesias number - 34 for 1 patient). Mean age - 6 years (6 months - 17 years). 76% of patients has CNS tumors, 9% lymphomas, 15% - soft tissue and other body tumors. 5 children with stem tumors has sevofluran anesthesia with mechanical ventilation, other has propofol with nasal oxygenation. In all patients ports or PICCs were used. For treatment time optimization, revolver-style anesthesia was implemented: 1st team waking up children after treatment, 2nd team provided anesthesia during treatment and in parallel, 3rd team started with sedation in anesthesia room, then all teams moving for new patients (Fig 1. Anesthesia cycle).
Results
Mean anesthesias number - 23 (20-32) per day. In 2 stem tumors patients during propofol anesthesia desaturation revealed and mechanical ventilation started. In 24 children radiation treatment was interrupted due to radiation-induced hydrocephalus, patients transferred to neurosurgery department for ventriculoperitoneal shunting and started again with radiotherapy. In 56 patients (15.5%), due to tumor decreasing and strong clinical psychologist support, on 15-20 fractions, we were able to refuse anesthesia and children continued proton therapy without sedation.
Fig 2. Treatment room
Conclusion
Implementation of pediatric anesthesia during proton therapy characterized by strong infrastructure creation (anesthesia rooms, awakening wards, patient trolleys with oxygen, monitoring and ventilator etc). For optimal treatment room time management it's critical to implement revolver-style patient anesthesia clinical way.