Using adjuvant radiotherapy for keloid scars: a patient and observer assessment study
PO-1564
Abstract
Using adjuvant radiotherapy for keloid scars: a patient and observer assessment study
Authors: Alice Alves1, Cláudia Sá2, Daniela Saraiva1, Pedro Soares1, João Casalta1, Gabriela Pinto1
1Centro Hospitalar Universitário São João, Radioterapia, Porto e Região, Portugal, Portugal; 2Instituto Portugues de Oncologia Lisboa, Radioterapia, Lisboa, Portugal
Show Affiliations
Hide Affiliations
Purpose or Objective
Keloid scar is a benign dermal condition that occurs due to excessive fibroblast activation, leading to an abnormal accumulation of collagen. These scars can be asymptomatic or associated with discomfort, pruritus, and pain, which may have a negative impact on quality of life. Due to a high recurrence rate, combined treatments might be considered. Adjuvant radiotherapy (RT) has shown to be effective in reducing local recurrence. This study aims to evaluate scar-related results after adjuvant RT, assessed by patients and clinicians, as well as efficacy on recurrence.
Material and Methods
Retrospective study including all patients with keloid scars undergoing surgical excision and adjuvant electron beam RT, from May 2016 to September 2022 at our hospital. The patient and observer scar assessment scale (POSAS) was used for all patients after RT, which assesses scar-related parameters (and overall score), scoring from 1 to 10. A RT dose of 18Gy/2fractions (9Gy/F), 7 days apart, was used, with 6MeV electrons and 3D conformal technique. All RT treatments began during the first 24h after surgery.
Data was analyzed using IBM SPSS Statistics v28. Spearman correlation was used for POSAS scale parameters, and reliability was assessed using standardized Cronbach’s alpha and its variation in item-by-item removal. Kaplan-Meier’s method was used for survival analysis. A significance of .05 was considered.
Results
32 patients and 36 keloid scars were evaluated, with a median follow-up of 3.5 years (interquartile range [IQR] of 8.25). Table 1 summarizes demographic, clinical and treatment data. No major adverse events were reported. Median for patient POSAS parameters varied between 1 and 3, with an overall score of 2 (IQR of 3, range 1-5). Significant correlations with overall score were observed for color (ρ=.35, p=.042), stiffness (ρ=.75, p<.001), thickness (ρ=.74, p<.001) and irregularity (ρ=.71, p<.001). Reliability for patient’s items was α=.796, with better contribution of stiffness, thickness and irregularity on item-by-item removal. Regarding observer parameters, medians varied between 1 and 2, with an overall score of 2 (IQR 1, range 1-5). All individual parameters showed significant correlations with overall score (ρ>.55, p<.001). Reliability for these items was α=.898, with better contribution of thickness, relief, pliability and area on item-by-item removal. There was no significant correlation between patient and observer overall score (ρ=.26, p=.14). Only one recurrence was observed, with a 1-year progression free survival of 93.8%.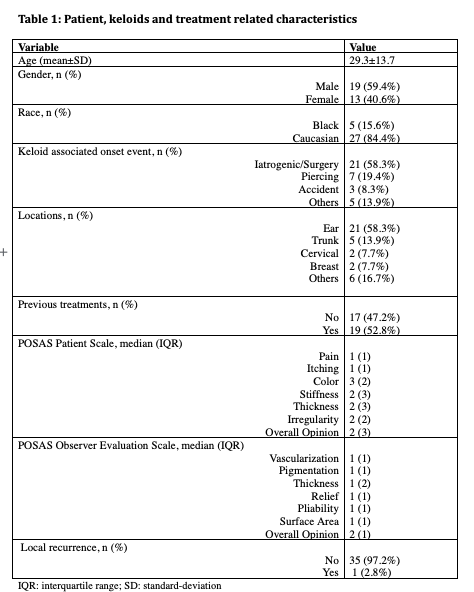
Conclusion
Our study showed that surgical excision combined with adjuvant RT is an excellent option, with good results assessed both by the patients and the clinicians, although their perspectives regarding results might differ. We also reported a very low recurrence rate, although a longer patient follow-up is required.